
any patient. The median time to urinary catheter removal
was 5.5 d and the median hospital stay was 6 d. For the
continence endpoint, we used two measures. For conti-
nence defined as 0 pads/d, 21.9% of patients in the ARVUS
group and 5.9% in the control group were continent at 24 h
after catheter removal. At the later time points, continence
rates for the ARVUS versus control groups were 43.8%
versus 11.8% at 2 wk (
p
= 0.005), 62.5% versus 14.7% at 4 wk
(
p
<
0.001), 68.8% versus 20.6% at 8 wk (
p
<
0.001), 75.0%
versus 44.1% at 6 mo (
p
= 0.013), and 86.66% versus 61.29%
at 12 mo (
p
= 0.04), respectively
( Table 2 ). A significant
improvement in continence was evident from the time of
catheter removal and at the 8-wk visit. We also evaluated
continence using the ICIQ-SF
( Table 2 ). The median ICIQ-SF
score at 24 h after catheter removal was 8.5 for the ARVUS
group and 13 for the control group (
p
= 0.008). At 2, 4, and
8 wk after catheter removal, the median scores were 7, 4.5,
and 4 for the ARVUS group, and 11, 10, and 8.5, respectively,
for the control group (
p
<
0.001 for all time points). Median
ICIQ-SF scores at 6 and 12 mo were 3 and 1 in the ARVUS
group, and 5.5 and 4, respectively, in the control group.
At 12 mo, six patients were still incontinent. For these
patients, further investigations included a 1-h standardised
pad test, a micturition diary, and a urodynamics study. One
patient in the ARVUS group had mixed stress and urge
incontinence. In the control group, two patients had stress
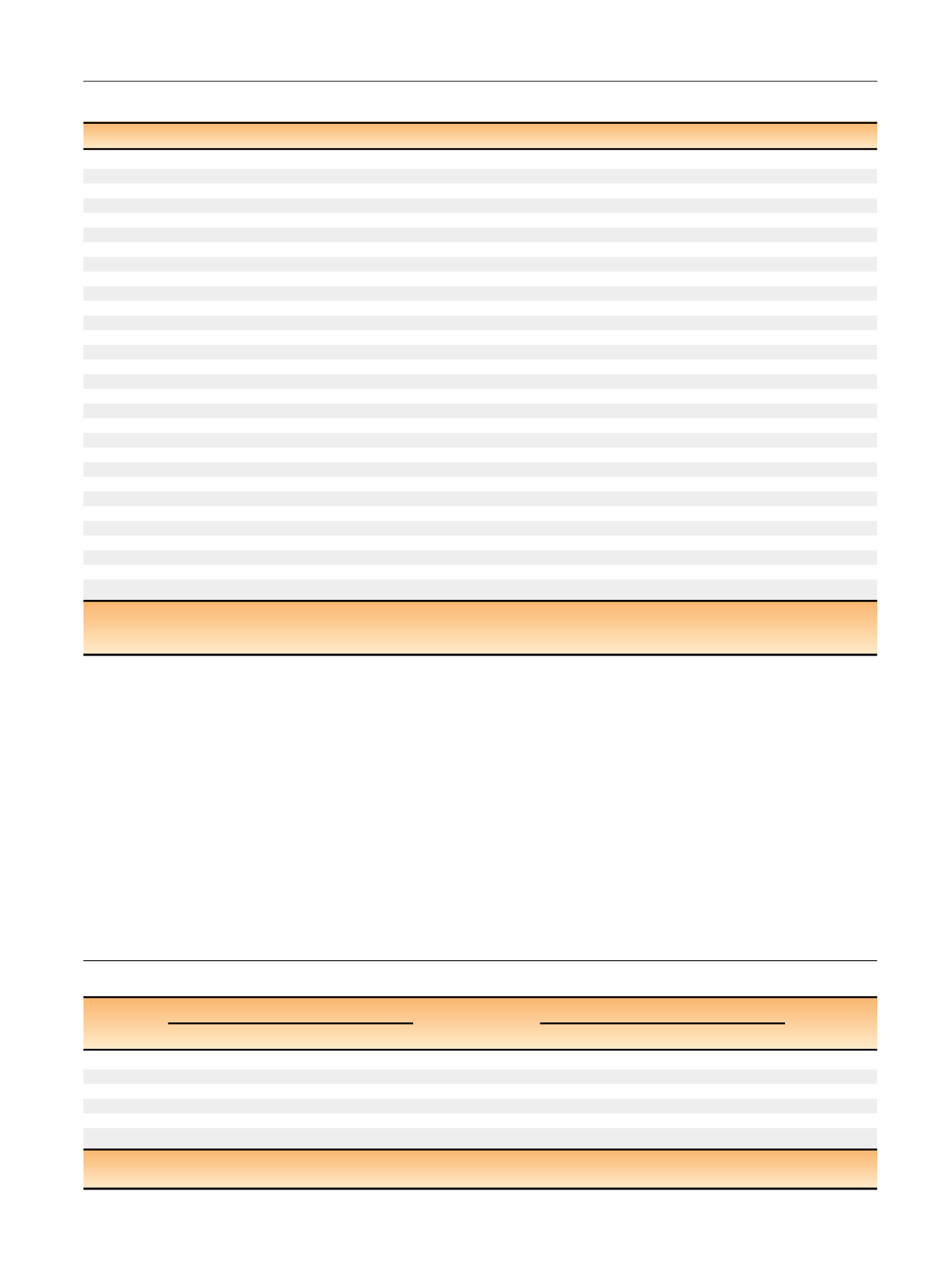
Table 2 – Continence data at various time points
Time
Patients achieving continence,
n
(%
) ap
value
Median ICIQ-SF score (5th–95th percentile)
p
value
Control group (
n
= 34)
ARVUS (
n
= 32)
Control group (
n
= 34)
ARVUS (
n
= 32)
24 h
2 (5.9)
7 (21.9)
0.079
13.0 (9.0–16.0)
8.5 (3.00–14.00)
0.008
2 wk
4 (11.8)
14 (43.8)
0.005
11.0 (8.0–14.0)
7.0 (3.00–9.00)
<
0.001
4 wk
5 (14.7)
20 (62.5)
<
0.001
10.0 (6.0–14.0)
4.5 (1.00–7.00)
<
0.001
8 wk
7 (20.6)
22 (68.8)
<
0.001
8.5 (4.0–12.0)
4.0 (1.00–7.00)
<
0.001
6 mo
15 (44.1)
24 (75.0)
0.013
5.5 (0.0–15.35)
3.0 (0.0–8.0)
<
0.001
12 mo
19 (61.3)
26 (86.7)
0.040
4.0 (0.0–16.0)
1.0 (0.00–9.00)
<
0.035
ICIQ-SF = International Consortium on Incontinence Questionnaire, short form; ARVUS = advanced reconstruction of vesicourethral support.
a
Continence defined as 0 pads/d.
Table 1 – Patient characteristics, perioperative data, and pathologic outcomes
Control group (
n
= 34)
ARVUS (
n
= 32)
p
value
Age (yr)
62.5 (61.0–68.0)
64.5 (56.0–67.0)
0.695
Body mass index (kg/m
2
)
28.0 (25.4–31.4)
27.7 (25.7–33.2)
0.959
ASA score
2.0 (1.0–2.0)
2.0 (1.0–2.0)
0.873
TRUS prostate volume (cm
3
)
32.5 (22.0–52.0)
35.0 (30.0–55.0)
0.397
Preoperative PSA (ng/ml)
5.7 (3.6–12.0)
7.3 (5.2–11.2)
0.060
D’Amico risk group
Low risk
15 (44.1)
13 (40.62)
0.999
Intermediate risk
12 (35.3)
12 (37.5)
High risk
7 (20.6)
7 (21.9)
IPSS score
5.0 (2.8–14.0)
5.5 (2.0–9.3)
0.374
IIEF-5 score
17.0 (13.3–21.0)
19.0 (13.5–21.0)
0.777
Console time (min)
76.5 (48.0–130.0)
78.0 (63.0–126.0)
0.559
Blood loss (ml)
140.0 (80.0–294.0)
145.0 (85.5–234.5)
0.146
Prostate size (g)
51.0 (42.0–64.0)
53.5 (48.0–64.0)
0.362
Middle lobe
2 (5.9)
2 (6.3)
0.999
Nerve sparing
Bilateral
23 (67.6)
20 (62.5)
0.647
Unilateral
5 (14.7)
6 (18.75)
None
6 (17.6)
6 (18.75)
Lymph node dissection
8 (23.52)
7 (21.9)
0.7661
Postoperative complications
Clavien grade 2
2 (5.8)
1 (3.1)
Clavien grade 3
0
1 (3.1)
Pathologic stage
pT2
23 (67.6)
20 (62.5)
0.797
pT3a
8 (23.52)
10 (31.25)
pT3b
3 (8.82)
2 (6.25)
Pathologic Gleason score
>
6
27 (79.4)
26 (81.3)
0.999
Positive surgical margins
5 (14.7)
4 (12.5)
0.999
Pathologic node-positive cancer
2 (5.9)
0 (0.0)
0.009
ARVUS = advanced reconstruction of vesicourethral support. ASA = American Society of Anesthesiologists; TRUS = transrectal ultrasound; PSA =
prostate-specific antigen; IPSS = International Prostate Symptom Score; IIEF = International Index of Erectile Function.
Data are presented as median (5th–95th percentile) for continuous variables and
n
(%) for categorical variables.
E U R O P E A N U R O L O G Y 7 1 ( 2 0 1 7 ) 8 2 2 – 8 3 0
827
















