
2.2.
Surgical technique
All patients underwent transperitoneal RARP. The criteria for NS surgery
were cT1–2a and Gleason score 7. The resection phase was the same for
both groups, similar to Mottrie et al.
[13] .Patient positioning and port
placement were standard and have been described by other authors
[14]. We used NS techniques if indicated (interfascial or at least
extrafascial); pedicles were treated using Hem-o-lok clips. We also tried
to preserve the maximum length of the urethra. In the case of large
middle prostate lobes, we had to reconstruct the bladder neck.
2.2.1.
Reconstruction phase
The reconstruction phase
( Fig. 1 )was performed in two ways. In the
control group, we sutured the Denonvilliers fascia and bladder to the
median dorsal raphe according to Rocco
[12], which was our standard
technique
( Fig. 2 A). In the ARVUS group, we used a new method of
sculpturing the pelvic floor muscles and an absorbable monofilament
barbed V-loc 2/0 suture, which we led first to the right, across the medial
bundles of the levator ani muscle, and then through the Denonvilliers
fascia
( Fig. 2B) without injuring the neurovascular bundles. We then led
the stitch over the bundles of the left medial levator ani and back to the
Denonvilliers fascia
( Fig. 2 C), tightened the structures together, and
finally led the end of the stitch under the urethra through the median
dorsal raphe and back through the detrusor under the bladder neck
through the retrotrigonal layer
( Fig. 2 D,E). In the last step, the needle was
passed through the bladder neck and urethra to align them
( Fig. 2 F). This
created a strong support for the anastomosis, which was supported by a
semi-circle of surrounding musculature, avoiding damage to the
neurovascular bundles.
2.2.2.
Anastomosis
The tension free anastomosis was created in both groups in the same
manner. We used two tied 3/0 monofilament fibres to create the
anastomosis, starting at the 5 or 6 o’clock position
( Fig. 3A), continuing
in both directions along the circumference, and then knotted at the
11–12 o’clock position
( Fig. 3 B).
2.2.3.
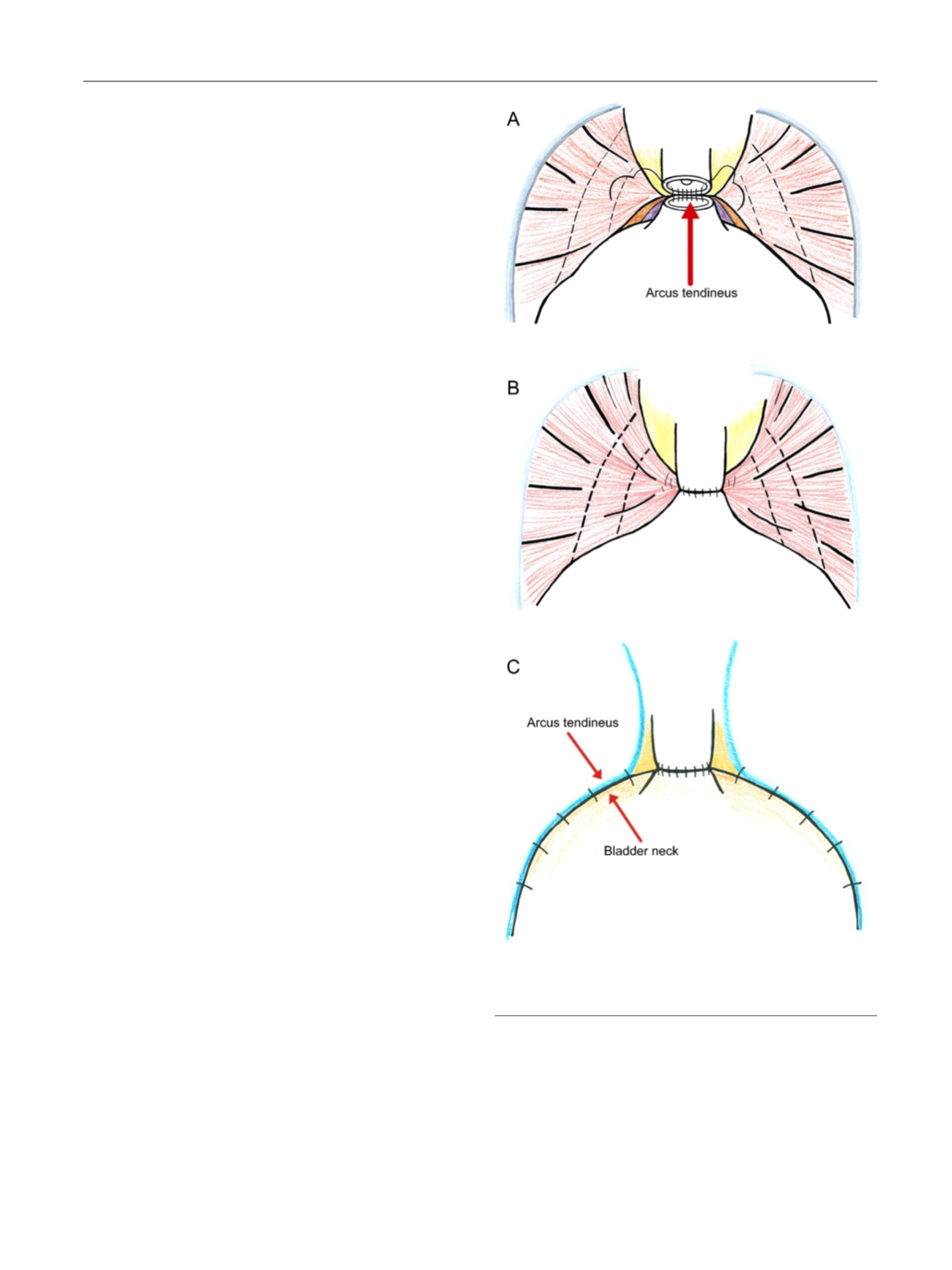
Reattachment of the arcus tendineus to the bladder neck
In both groups, after completion of the anastomosis, a further 3/0
monofilament stitch was used to suture the arcus tendineus to the
bladder neck
( Fig. 3 C), which was then fixed to the muscles of the pelvic
floor to reinforce the posterior and side support anastomosis.
2.2.4.
Extraction of the prostate, drainage, catheter removal, and
postoperative care
In both groups, the prostate was placed in an endobag and removed
through the opening after the camera port. A drain was placed next to the
anastomosis. The drain was removed on the second day after surgery;
the urinary catheter was removed on the fifth day if there were normal
findings on pelvic ultrasound (US). After catheter removal, we performed
US and checked for postvoid residuum. We performed a cystogramonly in
the case of urinary leakage (urine in the drainage sac or pathology revealed
by US). Patients in both groups were instructed to performKagel exercises,
which were not standardised. There was no rehabilitation programme. In
cases of persistent incontinence 12 mo after surgery, we added to the
automatic International Prostate SymptomScore (IPSS) a standardised 1-h
pad test, 3-d micturition diary, and urodynamics study to investigate
whether incontinence was due to an overactive bladder.
2.3.
Data collection
We compared demographic data and preoperative and postoperative
functional and oncologic results for the two groups. Recurrent cancer
was defined according to European Association of Urology guidelines as
two consecutive PSA values
>
0.2 ng/ml and rising
[15] .Complications
were recorded and evaluated using the Clavien-Dindo classification
[16]. Continence was assessed using the International Consortium on
Incontinence Questionnaire, short form (ICIQ-SF). Patients were also
asked about the number of pads used per day. Other evaluation forms
used were the IPSS and International Index of Erectile Function (IIEF-5).
We collected preoperative IPSS and IIEF-5 data. Postoperatively, the IPSS
and ICIQ-SF questionnaires were completed at 24 h after urinary
catheter removal (responses 2 and 3 to the first ICIQ-SF question could
[(Fig._3)TD$FIG]
Fig. 3 – (A) The beginning of the tension-free anastomosis. (B) Frontal
view of the completed tension-free anastomosis. (C) The arcus
tendineus is sutured to the bladder neck in both groups.
E U R O P E A N U R O L O G Y 7 1 ( 2 0 1 7 ) 8 2 2 – 8 3 0
825
















