
1.
Introduction
Radical prostatectomy (RP) for localised prostate cancer has
excellent oncologic results and a low rate of complications
[1,2]. However, functional outcomes in terms of continence,
and erection still lag behind,markedly reducing the quality of
everyday life for patients, especially those who are younger
and more active
[3]. The proportion of continent patients at
12 mo after surgery ranges from 69% to 96%
[4] .Noteworthy
is the relatively long duration to achieve continence. The
disparities in the literature result from various definitions of
continence and measurement methods (questionnaires,
number of pads, pad test). A number of factors have been
identified for postprostatectomy incontinence (PPI), includ-
ing patient characteristics (body mass index, age, prostate
volume, and comorbidities), surgeon experience, and surgical
precision
[5]. No effect of pelvic floor muscle exercise before
surgery on PPI has been conclusively demonstrated
[6].
The advent of minimally invasive methods has facilitated
new surgical techniques, ways of resection, and especially
the reconstruction phase after RP, aimed at improving
functional results without impairing early oncologic out-
comes
[7] .This allows us to adjust the anatomical and
functional relationships in the pelvis after removal of the
prostate to ameliorate PPI and reduce the time to achieve
complete continence. A number of papers and several
reviews with very promising results in this direction have
been published. The time to complete continence has been
gradually reduced to 3-6 months, resulting in clear benefits
for patients
[5] .Hence, it is now possible to refine the
surgical technique in order to reduce the incidence of PPI,
rather than resolve the PPI when it occurs
[8].
There are a number of operating procedures and
techniques for improving continence after RARP: preserva-
tion of the bladder neck, nerve-sparing (NS) techniques,
preserving maximum length of the urethra, preserving the
puboprostatic ligament and endopelvic fascia, posterior
rhabdosphincter reconstruction, anterior reconstruction,
and suture of the arcus tendineus to the bladder neck
[9,10] .This study was motivated by a new technique for
performing the reconstructive phase of RARP, involving
suture of the pelvic floor muscles to create a dynamic
semicircular support for the urethra
[11] .This technique has
been adopted in operations without the use of NS techniques
with excellent results for continence. This inspired us to use
the principle to devise our own method for advanced
reconstruction of vesicourethral support (ARVUS) obviating
damage to the neurovascular bundles, creating support for
the anastomosis, fixing the arcus tendineus to the bladder
with the medial levator ani, and correcting the functional-
anatomical relations after RP. Here we present the first
results for this method in comparison to the standard
posterior reconstruction method of Rocco that we have
routinely used at our institution since 2009
[12].
2.
Patients and methods
2.1.
Study population and design
This was a prospective, randomised study involving 66 consecutive
patients presenting to our Department of Urology for RARP from June to
September 2014. The inclusion criterion was localised prostate cancer
(cT1–2N0M0). Exclusion criteria were: patients not suitable for RARP or
any neoadjuvant hormonal treatment, prior radiation therapy, no
transurethral resection of the prostate, and previous history of urethral
stricture and urinary incontinence. Patients were randomised to two
groups using the online software QuickCalcs (GraphPad Software, San
Diego, CA, USA) with blinding for group allocation. The study coordinator
informed the surgeon of the randomisation outcome before surgery. The
other members of the team involved in the study did not know the
randomisation results. The ethics committee of the University Hospital
had strong objections to blinded procedures in patients, but eventually
approved the blinding protocol. This was done at the outset of the study.
The patients gave their written informed consent. One surgeon (V.S.)
with experience of more than 800 RARPs performed the surgeries. This
innovative technique had already been performed in 15 patients who
were not included in this study.
Conclusions:
The ARVUS technique yielded better urinary continence results than standard
posterior reconstruction, with no negative impact on erectile function, complication rate, or
oncologic outcome. External validation is warranted before clear recommendations can be
made.
Patient summary:
We showed that postprostatectomy incontinence can be assuaged using
a new technique for vesicourethral anastomosis reconstruction during robot-assisted
radical prostatectomy (RARP). This could significantly improve the quality of life of patients
after RARP. More studies are needed to support our results.
#
2016 European Association of Urology. Published by Elsevier B.V. All rights reserved.
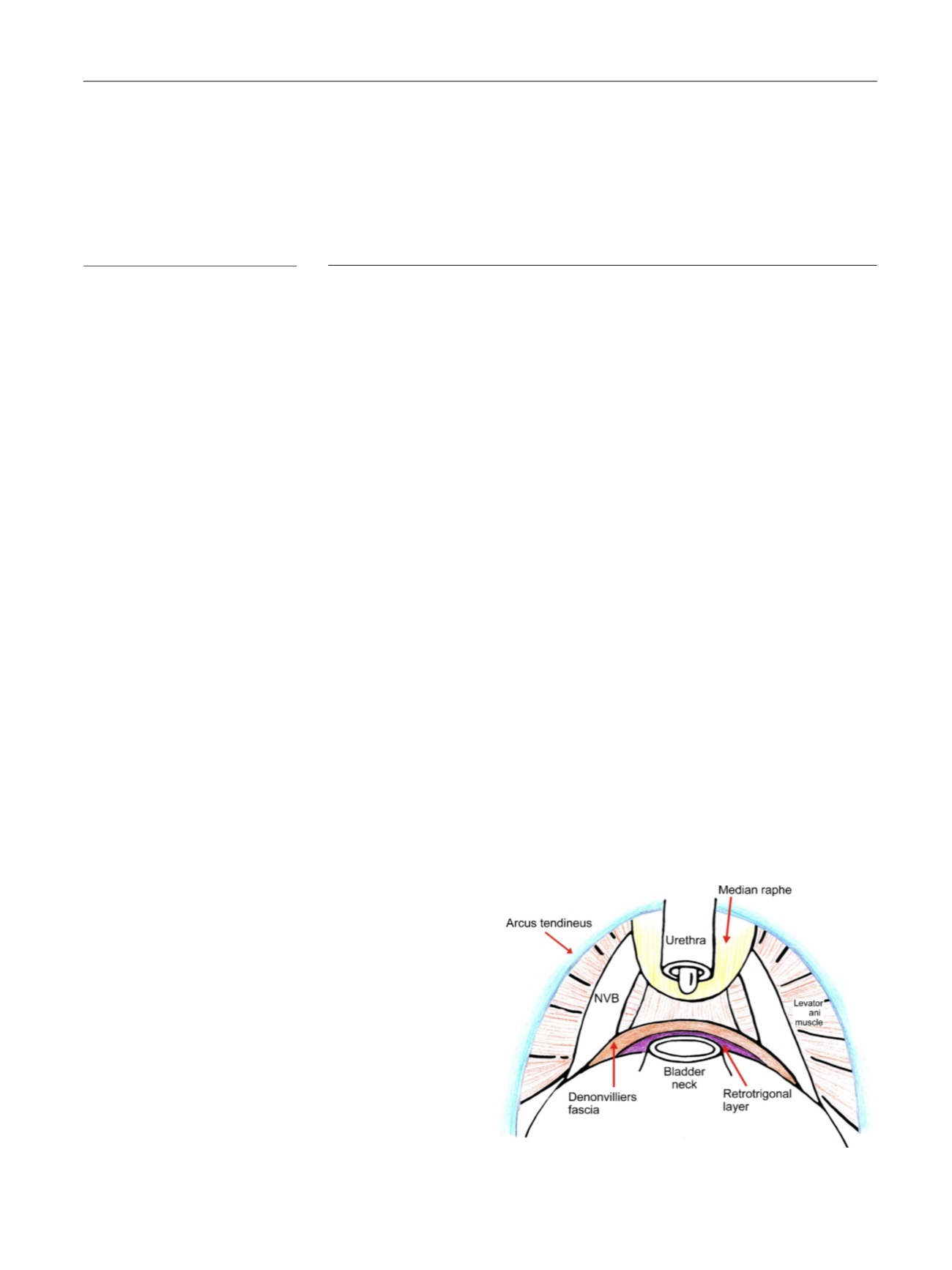
[(Fig._1)TD$FIG]
Fig. 1 – Anatomic structures involved in the reconstruction phase.
NVB = neurovascular bundle.
E U R O P E A N U R O L O G Y 7 1 ( 2 0 1 7 ) 8 2 2 – 8 3 0
823
















