
Adjusted pairwise comparisons of prognostic Gleason grade
group were significantly different with the exception
of group II versus group III (
p
= 0.74) and group IV versus
group V (
p
= 0.32).
Among men treated with RP (
n
= 5058), the unadjusted
risks of PCSM and metastatic progression were successively
higher by pathologic prognostic Gleason categories
( Tables 2 and 4). On multivariable Cox proportional hazards
regression analysis, relative to grade group I, all were
independently associated with risk of PCSM (
p
<
0.01).
Similar associations were observed for the risk of bone
metastatic progression among prognostic Gleason categories
( Table 4 ).
Unadjusted outcomes based on extended Gleason grade,
reflecting the effect of uncoupling for prognostic grade
group V (patterns 4 + 5, 5 + 4, and 5 + 5) are depicted in
Figure 2[7_TD$DIFF]
and
Table 3[2_TD$DIFF]
. Adjusted pairwise comparison of
pattern 4 + 5 and pattern 5 + 4,
[3_TD$DIFF]
revealed no significant
difference
[8_TD$DIFF]
in risk of PCSM. In the subset of men treated with
RP, the risk of PCSM compared to group I also significantly
differed between the three conventional Gleason scores
contained within prognostic group V (
p
<
0.01;
Table 3).
[4_TD$DIFF]
283 men experienced metastatic progression. Figures 1B
and 2B showKaplan-Meier survival plots of the time to bone
metastasis by prognostic grade group. Prognostic grade
group was associated with risk of bone metastasis. Relative
to grade group I, in unadjusted analysis the prognostic grade
group was associated with the risk of bone metastasis
(
p
<
0.01;
Table 4). Among the prognostic categories,
adjusted pairwise comparisons revealed significant differ-
ences, with the exception of group II versus group III
(
p
= 0.81), and group IV versus group V (
p
= 0.48). Adjusted
pairwise comparisons among patterns 4 + 5, 5 + 4, and 5 + 5
revealed no significant differences (Supplementary Table 1).
[9_TD$DIFF]
Outcomes of by extended Gleason grade patterns are
presented in
Table 54.
Discussion
Comprehensible reporting of PCa histologic grades is likely
to have an impact on a disease characterized by diversity in
biology, clinical outcomes, management choices, and
quality of information
[15–17] .This may be particularly
meaningful at the lower end of the spectrum, where high
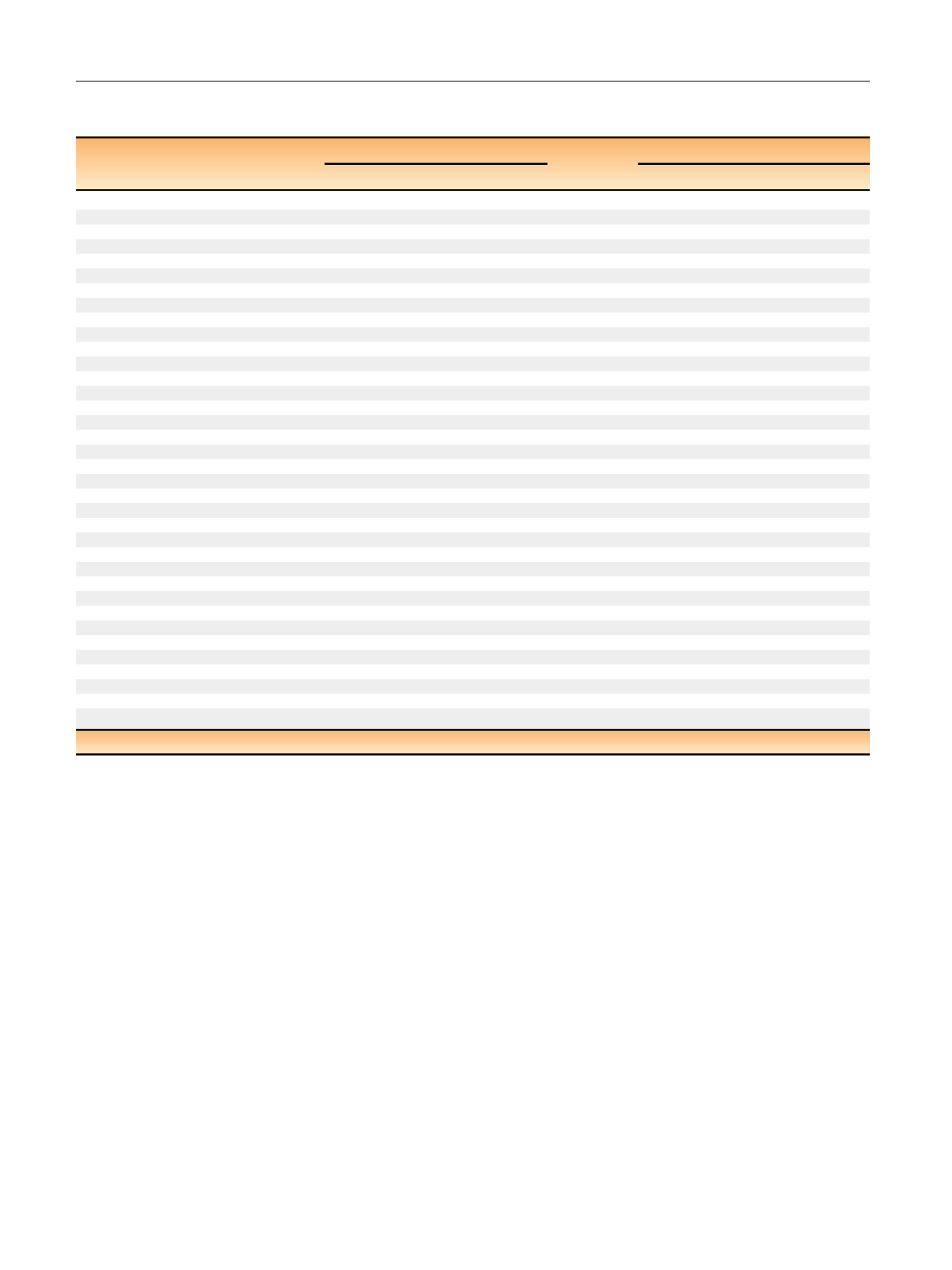
Table 4 – Results of a Cox proportional hazards model examining factors associated with risk of bone metastasis among men within the
CaPSURE study based on proposed prognostic Gleason grade groupings
Independent variable
Biopsy grade (all treatments)
Surgical grade (RP only)
p
value
HR (95% CI)
p
value
HR (95% CI)
Univariate model
Gleason grade
I (2–6) (reference)
<
0.01
1.00
<
0.01
1.00
II (3 + 4)
2.20 (1.59–3.04)
1.76 (1.04–2.97)
III (4 + 3)
2.56 (1.72–3.82)
2.38 (1.21–4.68)
IV (8)
6.03 (4.33–8.40)
6.70 (3.92–11.4)
V (9–10)
7.31 (4.93–10.8)
9.66 (5.04–18.5)
Multivariate model
Gleason grade
I (2–6) (reference)
<
0.01
1.00
<
0.01
1.00
II (3 + 4)
2.08 (1.47–2.95)
1.96 (1.14–3.39)
III (4 + 3)
2.20 (1.41–3.43)
3.06 (1.47–6.38)
IV (8)
4.21 (2.90–6.13)
7.07 (4.02–12.4)
V (9–10)
4.98 (3.24–7.64)
8.04 (4.13–15.7)
Year of diagnosis
<
0.01
0.93 (0.90–0.96)
<
0.01
0.88 (0.83–0.92)
Age at diagnosis per 10 yr
0.13
1.16 (0.96–1.39)
0.42
1.14 (0.83–1.57)
Race
Other (reference)
0.09
1.00
0.05
1.00
African American
0.50 (0.25–0.99)
0.37 (0.10–1.45)
Caucasian
1.02 (0.72–1.44)
1.49 (0.71–3.13)
Log PSA at diagnosis
1.45
1.25 (1.69–1.45)
<
0.01
1.53 (1.17–2.00)
Clinical T stage
T1 (reference)
<
0.01
1.00
0.02
1.00
T2
1.59 (1.16–2.18)
1.43 (0.87–2.36)
T3/4
2.86 (1.82–4.50)
3.15 (1.45–6.84)
Primary treatment
RP (reference)
0.07
1.00
Brachytherapy
0.63 (0.35–1.11)
External beam radiation
1.21 (0.85–1.73)
Hormonal therapy
0.93 (0.60–1.42)
AS/WW
1.55 (0.91–2.64)
Clinical site
Academic center (reference)
0.40
1.00
0.01
1.00
Community-based practice
1.14 (0.65–2.00)
0.67 (0.32–1.41)
Veterans Affairs center
1.77 (0.74–4.24)
3.14 (0.90–11.0)
x
2
likelihood ratio
281.6
149.3
RP = radical prostatectomy; HR = hazard ratio; CI = confidence interval; PSA = prostate-specific antigen; AS = active surveillance; WW = watchful waiting.
E U R O P E A N U R O L O G Y 7 1 ( 2 0 1 7 ) 7 5 0 – 7 5 9
756
















