
used to examine the independent associations between Gleason grade
(modeled as an ordinal) and outcomes, adjusting for age and PSA at
diagnosis (log-transformed to normalize distribution), hospital setting
(academic, vs community or Veterans Affairs), pathologic T stage, and
surgical margin status, and including pairwise comparisons between
Gleason grade categories. Covariates were selected a priori and tested for
between-item correlation. Statistical significance was set at
p
<
0.05. All
analyses were performed using SAS 9.4 for Windows (SAS Institute, Cary,
NC, USA).
3.
Results
The primary cohort consisted of 10 529 men whose primary
management consisted of RP, EBRT, BT, ADT, or AS/WW.
These included 6776men (64%) in grade group I; 1773 (17%)
in group II; 955 (9%) in group III; 636 (6%) in group IV; and
389 (4%) in group V. Men treated with RP were younger
(mean age 61.6 yr) than those who underwent BT
monotherapy (mean 68.0 yr), EBRT (mean 70.1 yr), primary
ADT (73.0), or AS/WW (mean 71.4;
p
<
0.01. Median follow-
up after treatment for patients not experiencing PCSM was
81 mo (interquartile range 40–127). Complete baseline
clinical and demographic characteristics are presented in
Table 1.
A total of 510 men experienced death due PCa. Relative
to grade group I, the unadjusted risk of PCSM was
significantly higher among successive prognostic category
groups (
p
<
0.01;
Table 2). The Kaplan-Meier survival plot
stratified by grade group is depicted in
Figure 1. In a
multivariate Cox proportional hazards regression model
adjusted for age, clinical stage, PSA, treatment modality,
year of diagnosis, race, and hospital setting (clinical site),
Gleason grade group was independently associated with
risk of PCSM. In addition, PSA at diagnosis, clinical T stage,
and receipt of EBRT, primary ADT, or AS/WW were
significantly associated with risk of PCSM
( Table 2).
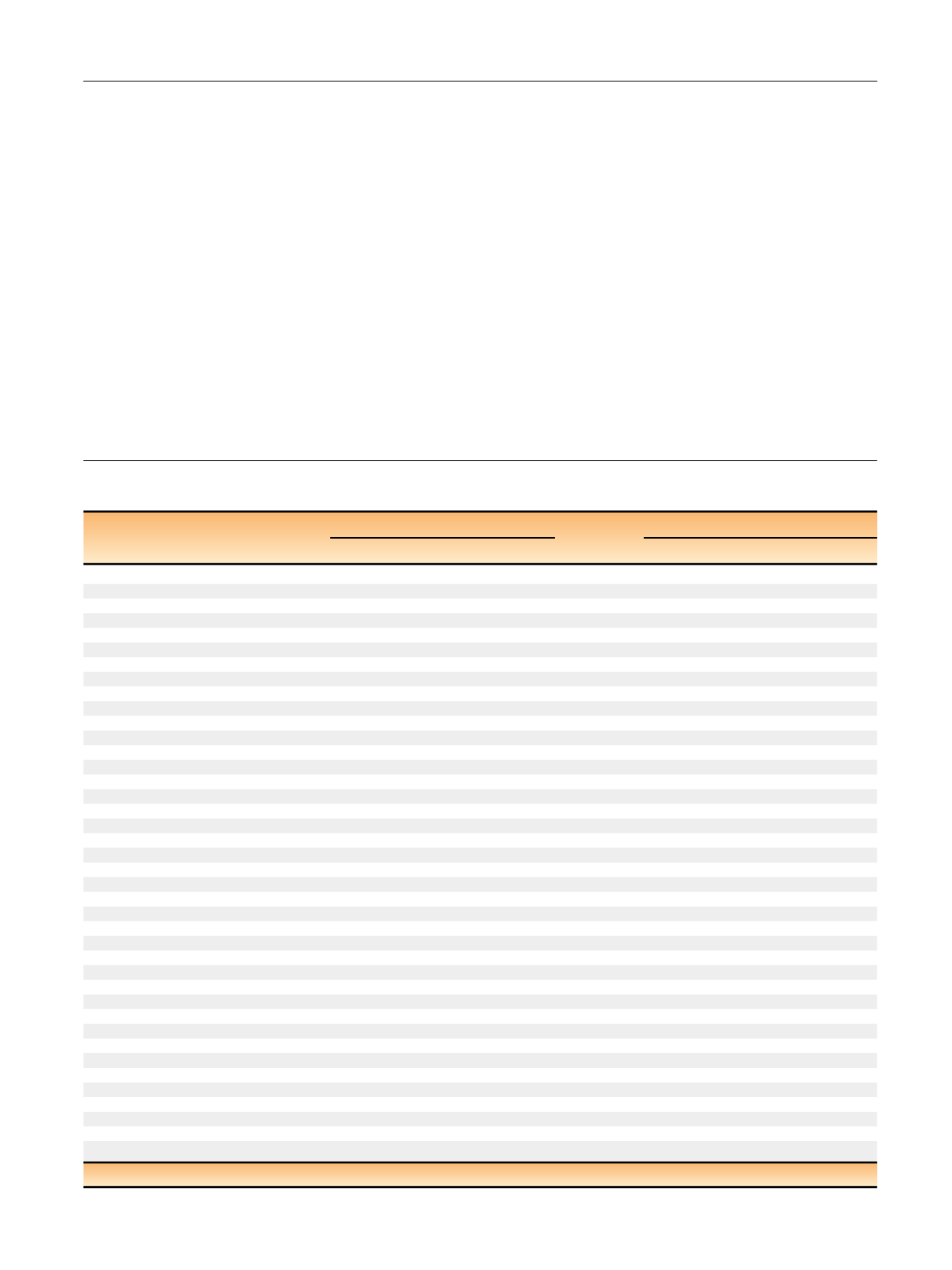
Table 3 – Results from a Cox proportional hazards model examining factors associated with risk of death from prostate cancer among men
within the CaPSURE study based on extended prognostic Gleason grade groupings
Independent variable
Biopsy grade (all treatments)
Surgical grade (RP only)
p
value
HR (95% CI)
p
value
HR (95% CI)
Univariate model
Gleason grade
2–6 (reference)
<
0.01
1.00
<
0.01
1.00
3 + 4
2.39 (1.87–3.07)
1.93 (1.17–3.17)
4 + 3
2.97 (2.19–4.02)
2.66 (1.39–5.06)
8
7.00 (5.48–8.93)
6.13 (3.51–10.7)
4 + 5
8.11 (5.58–11.8)
11.4 (6.34–20.6)
5 + 4
11.1 (6.58–18.8)
13.2 (5.53–31.7)
10
17.3 (9.63–31.1)
31.1 (9.52–102.)
Multivariate model
Gleason grade
2–6 (reference)
<
0.01
1.00
<
0.01
1.00
3 + 4
1.91 (1.45–2.52)
1.88 (1.10–3.22)
4 + 3
2.02 (1.44–2.84)
2.32 (1.15–4.69)
8
4.28 (3.24–5.65)
5.23 (2.86–9.59)
4 + 5
5.38 (3.55–8.15)
7.85 (4.01–15.4)
5 + 4
4.84 (2.65–8.83)
13.9 (5.71–33.9)
10
8.85 (4.83–16.2)
19.0 (5.03–71.7)
Year of diagnosis
0.02
0.97 (0.95–0.99)
0.01
0.93 (0.88–0.99)
Age at diagnosis per 10 yr
0.75
0.98 (0.85–1.12)
0.18
1.24 (0.91–1.69)
Race
Other (reference)
<
0.01
1.00
0.04
1.00
African American
0.59 (0.39–0.91)
0.36 (0.09–1.42)
Caucasian
0.67 (0.52–0.85)
1.62 (0.75–3.51)
Log PSA at diagnosis
<
0.01
1.51 (1.36–1.68)
0.07
1.31 (0.98–1.76)
Clinical T stage
T1 (reference)
<
0.01
1.00
0.07
1.00
T2
1.23 (0.98–1.55)
1.52 (0.92–2.52)
T3/4
1.71 (1.21–2.42)
2.71 (1.13–6.51)
Primary treatment
RP (reference)
<
0.01
1.00
Brachytherapy
1.39 (0.93–2.07)
External beam radiation
1.90 (1.43–2.53)
Hormonal therapy
2.52 (1.85–3.44)
AS/WW
2.42 (1.58–3.73)
Clinical site
Academic center (reference)
<
0.01
1.00
<
0.01
1.00
Community-based practice
2.69 (1.47– 4.94)
2.03 (0.74– 5.59)
Veterans Affairs center
2.13 (0.93–4.87)
11.5 (2.99–44.1)
x
2
likelihood ratio
533.6
135.4
RP = radical prostatectomy; HR = hazard ratio; CI = confidence interval; PSA = prostate-specific antigen; AS = active surveillance; WW = watchful waiting.
E U R O P E A N U R O L O G Y 7 1 ( 2 0 1 7 ) 7 5 0 – 7 5 9
755
















