
rates of treatment occur among those with Gleason
score
<
3 + 4 disease
[18] .The prospect of removing
historical vestiges within the Gleason scale (ie, sums 2–5)
has long been advanced as one response to the over-
detection and overtreatment challenge tied to population-
based PSA screening and appears to yield greater patient
comfort in focus groups of men with PCa
[19] .We evaluated the ability of this prognostic Gleason grade
grouping system to predict risk of downstream PCa
endpoints in a large, diverse cohort of men within the
CaPSURE study using both biopsy and pathologic Gleason
score. The prognostic grade grouping system offered
incremental prediction of risk of PCSM, with an unadjusted
hazard ratio ranging from 2.4 to 9.2. Among the subgroup of
men with biopsy Gleason sums 9–10 (Group V), we
observed distinctions in the hazard ratio for PCSM relative
to group I that ranged from 8.3 (Gleason 4 + 5) to 16.9
(Gleason 5 + 5). Moreover, all uncensored patients in the
Gleason 5 + 5 category had succumbed to their disease at
last follow-up, while long-term survival remained above
50% at 15-yr follow-up among those with patterns 5 + 4 at
initial biopsy.
Several recent publications have examined the effect of
the prognostic Gleason grade groups on outcome after
definitive treatment with limited clinical follow-up. Epstein
and colleagues
[11]reported on 20 845 men treated with RP
across five academic institutions and followed for a median
of 3.0 yr, and 5501 men treated with radiation at two
centers followed for a median of 3.1 yr, for whom the
prognostic Gleason scoring system discriminated the risk of
biochemical recurrence. Reporting of a five-level system
improved the prediction of biochemical recurrence risk
from pre-RP biopsy, post-RP pathology, and pre-RT biopsy
Gleason score. In addition, two recent publications exam-
ining the risk of PCSM in the context of conservative
management and radiotherapy revealed strong associations
between prognostic grade group and downstream outcome
[9,12].
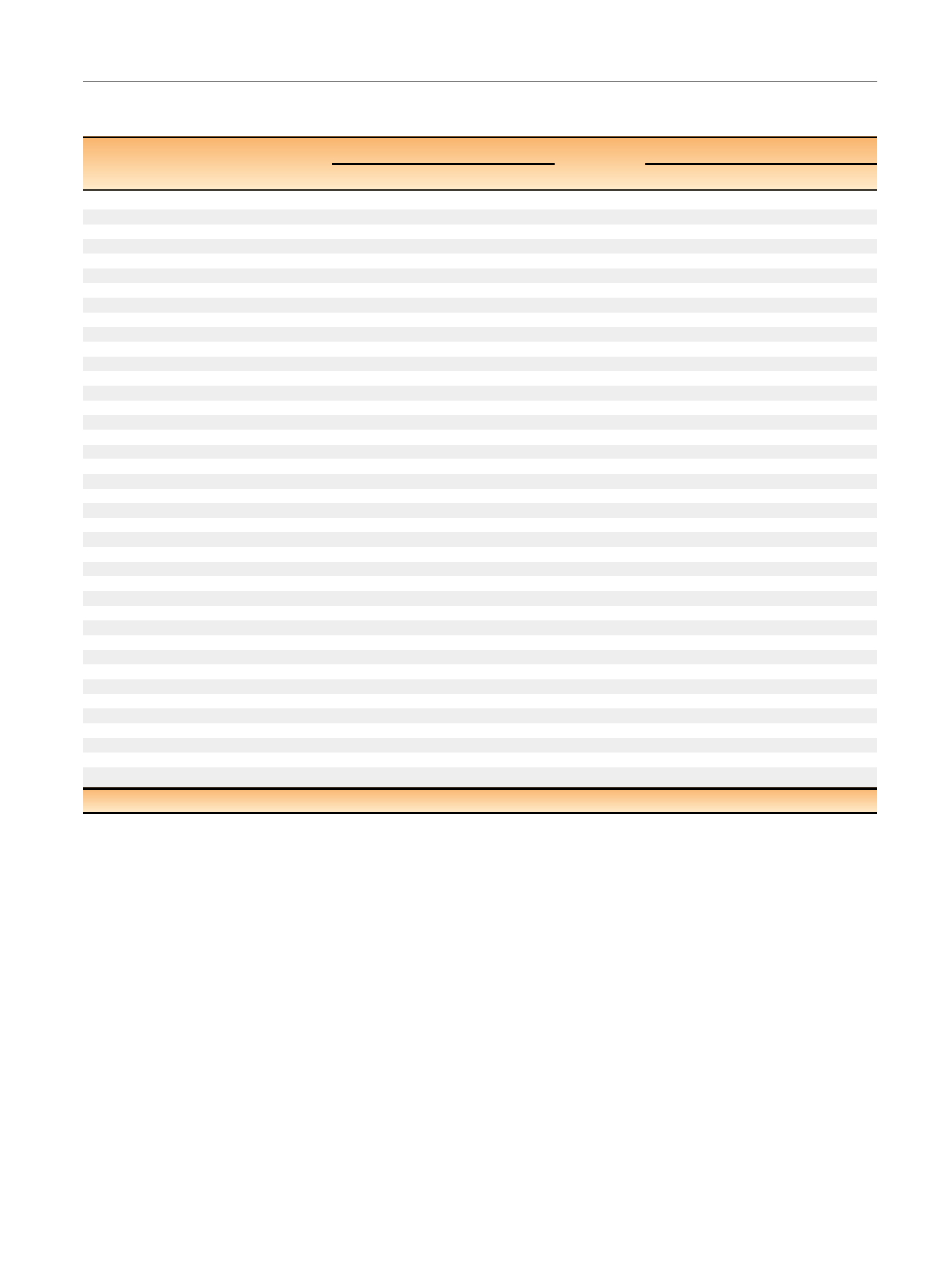
Table 5 – Results for a Cox proportional hazards model examining factors associated with risk of bone metastasis among men in the
CaPSURE study based on extended prognostic Gleason grade grouping
Independent variable
Biopsy grade (all treatments)
Surgical grade (RP only)
p
value
HR (95% CI)
p
value
HR (95% CI)
Univariate model
Gleason grade
2–6 (reference)
<
0.01
1.00
<
0.01
1.00
3 + 4
2.20 (1.59–3.05)
3.22 (1.66–6.26)
4 + 3
2.57 (1.72–3.82)
5.50 (2.55–11.9)
8
6.04 (4.33–8.41)
13.3 (6.63–26.8)
4 + 5
7.87 (4.84–12.8)
14.0 (6.04–32.2)
5 + 4
7.03 (3.09–16.0)
31.7 (12.2–82.5)
10
8.33 (3.07–22.6)
91.2 (30.0–277)
Multivariate model
Gleason grade
2–6 (reference)
<
0.01
1.00
<
0.01
1.00
3 + 4
2.08 (1.46–2.95)
2.99 (1.46–6.10)
4 + 3
2.19 (1.40–3.41)
5.28 (2.34–12.0)
8
4.14 (2.84–6.02)
11.3 (5.39–23.9)
4 + 5
6.23 (3.67–10.6)
11.7 (4.83–28.4)
5 + 4
4.47 (1.93–10.4)
29.9 (11.2–79.9)
10
6.16 (2.22–17.1)
43.7 (12.5–153.)
Year of diagnosis
<
0.01
0.93 (0.90–0.96)
<
0.01
0.89 (0.84–0.95)
Age at diagnosis per 10 yr
0.09
1.18 (0.98–1.43)
0.70
1.07 (0.76–1.51)
Race
Other (reference)
0.11
1.00
0.04
1.00
African American
0.51 (0.26–1.01)
0.56 (0.13–2.36)
Caucasian
1.00 (0.71–1.42)
2.19 (0.89–5.39)
Log PSA at diagnosis
<
0.01
1.44 (1.24–1.68)
0.11
1.31 (0.94–1.82)
Clinical T stage
T1 (reference)
<
0.01
1.00
<
0.01
1.00
T2
1.60 (1.17–2.19)
1.16 (0.65–2.06)
T3/4
3.15 (2.00–4.96)
3.55 (1.51–8.33)
Primary treatment
RP (reference)
0.05
1.00
Brachytherapy
0.62 (0.35–1.10)
External beam radiation
1.24 (0.87–1.76)
Hormonal therapy
0.90 (0.59–1.39)
AS/WW
1.53 (0.90–2.62)
Clinical site
Academic center (reference)
0.45
1.00
<
0.01
1.00
Community-based practice
1.19 (0.67–2.10)
0.85 (0.38–1.90)
Veterans Affairs center
1.74 (0.73–4.18)
5.60 (1.57–20.0)
x
2
likelihood ratio
284.5
157.5
RP = radical prostatectomy; HR = hazard ratio; CI = confidence interval; PSA = prostate-specific antigen; AS = active surveillance; WW = watchful waiting.
E U R O P E A N U R O L O G Y 7 1 ( 2 0 1 7 ) 7 5 0 – 7 5 9
757
















