
prospectively tracks clinical characteristics, treatment, relapse, survival,
and quality-of-life outcomes for men with PCa
[13]. CaPSURE comprises
43 sites, including 36 community-based practices, three academic
centers, and four US Veterans Affairs medical centers. The study is
managed under institutional review board supervision, with all patients
providing informed consent for research.
Selected patients were diagnosed with nonmetastatic disease and
underwent initial primary management with RP, external beam
radiation therapy (EBRT), brachytherapy (BT), primary androgen
deprivation (ADT), or active surveillance/watchful waiting (AS/WW).
We identified 14 862 men with PCa enrolled in the CaPSURE study
between 1995 and 2014. Of these, 410 patients (3%) were excluded
owing to positive lymph nodes, metastatic or clinical stage T4 disease at
enrollment; 1802 (12%) were excluded owing to primary treatment
outside of prespecified modalities, including 156 (1%) who had delayed
primary RP, 531 (3.6%) treated with cryotherapy, 331 (2.2%) who did not
receive treatment but were not classified as management with AS, and
783 (5.3%) who received other unspecified treatment or for whom
treatment data were incomplete. An additional 2121 men (14%) were
excluded because of incomplete data on initial biopsy Gleason score.
Thus, 10 529 patients were included in our analysis.
The primary outcome was risk of PCSM, and the primary indepen-
dent variable was the prognostic Gleason grade grouping system
proposed by the group from Johns Hopkins as presented at the
2014 International Society of Urological Pathology (ISUP) consensus
conference on Gleason grading of prostatic carcinoma
[5]. PCSM was
defined as death as direct result of PCa. Development of bone metastasis
was defined by the presence of a positive bone scan, receipt of irradiation
to bone, or explicit identification by the provider in clinical staging.
Gleason grade categories at first positive biopsy and at RP were
evaluated as
<
3 + 4 = 7 (I); 3 + 4 (II); 4 + 3 (III); 4 + 4 (IV); or 9–10 (V).
Gleason scores 3 + 5 and 5 + 3 were included in category IV, consistent
with prior publications
[11]. Other independent variables of interest
included age, race, clinical characteristics at diagnosis (year, prostate-
specific antigen [PSA], T stage), findings at surgical pathology (stage,
margin status), and disease risk as measured using the CAPRA (UCSF
Cancer of the Prostate Clinical Risk Assessment) score
[14]. Modeling
was repeated in a secondary analysis in which we extended the Gleason
categories to 3 + 3, 3 + 4, 4 + 3, 4 + 4, 4 + 5, 5 + 4, and 5 + 5. Risk of bone
metastasis was regarded as a secondary endpoint and modeled similarly.
Independent and exposure variables were described using mean,
median, and frequency tables. Clinical and surgical pathology char-
acteristics were compared by Gleason grade category using analysis of
variance. The unadjusted risk of each outcome event was assessed using
Kaplan-Meier curves, and rates were compared by Gleason grade
category with the log-rank test. Cox proportional hazards regression was
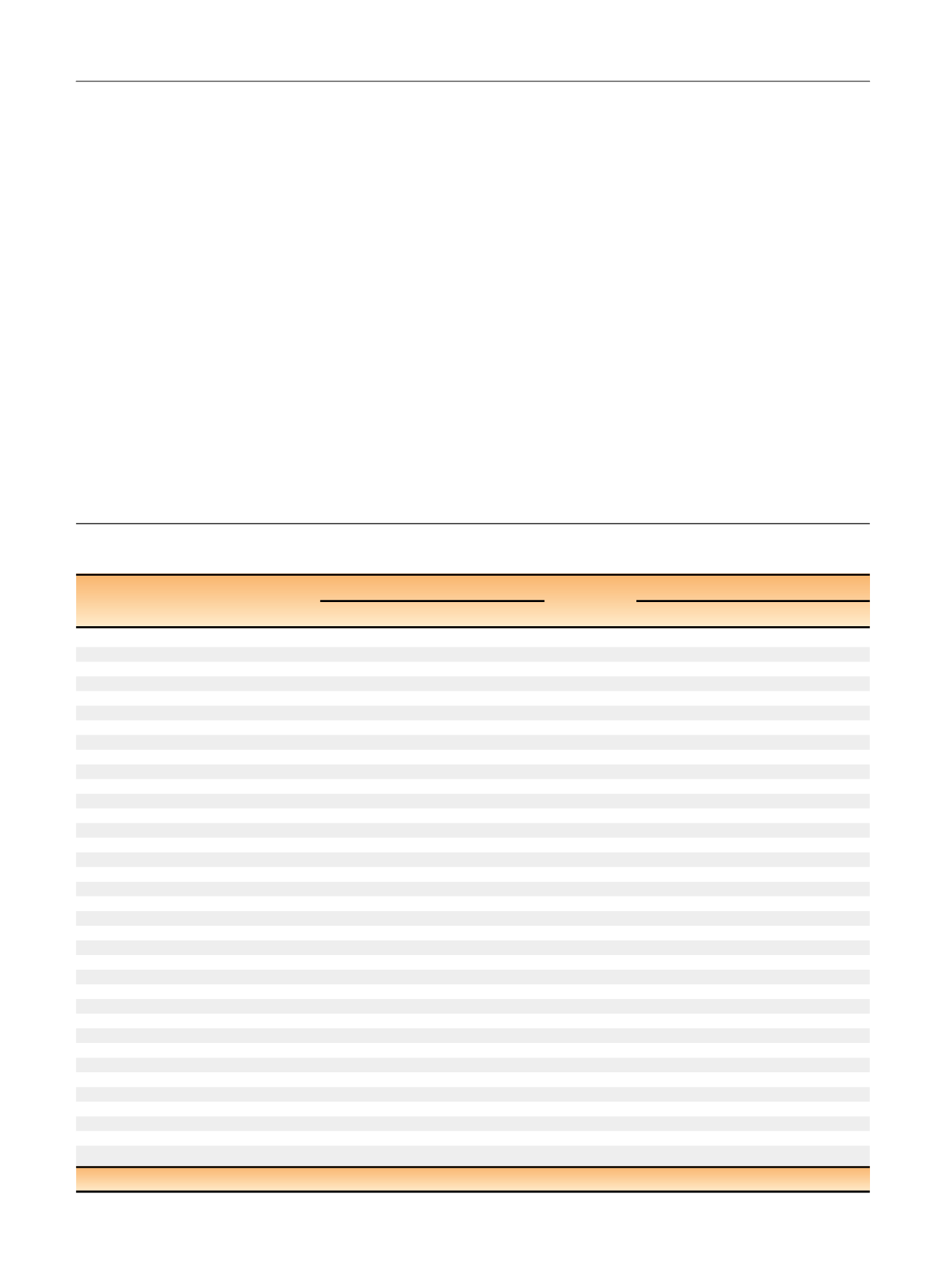
Table 2 – Results from a Cox proportional hazards model examining factors associated with risk of death from prostate cancer among men
in the CaPSURE study based on proposed prognostic Gleason grade groupings
Independent variable
Biopsy grade (all treatments)
Surgical grade (RP only)
p
value
HR (95% CI)
p
value
HR (95% CI)
Univariate model
Gleason grade
I (2–6) (reference)
<
0.01
1.00
<
0.01
1.00
II (3 + 4)
2.39 (1.86–3.06)
1.93 (1.17–3.17)
III (4 + 3)
2.96 (2.19–4.00)
2.65 (1.39–5.06)
IV (8)
6.98 (5.47–8.91)
6.12 (3.50–10.7)
V (9–10)
9.12 (6.90–12.0)
12.6 (7.56– 20.9)
Multivariate model
Gleason grade
I (2–6) (reference)
<
0.01
1.00
<
0.01
1.00
II (3 + 4)
1.92 (1.45–2.53)
1.91 (1.11–3.27)
III (4 + 3)
2.04 (1.45–2.85)
2.36 (1.17–4.77)
IV (8)
4.35 (3.29–5.75)
5.25 (2.87–9.62)
V (9–10)
5.15 (3.75–7.09)
9.46 (5.38–16.7)
Year of diagnosis
0.02
0.97 (0.95–1.00)
<
0.01
0.92 (0.88–0.98)
Age at diagnosis (per 10 yr)
0.55
0.96 (0.84–1.10)
0.30
1.18 (0.87–1.59)
Race
Other (reference)
<
0.01
1.00
0.07
1.00
African American
0.59 (0.39–0.90)
0.36 (0.09–1.37)
Caucasian
0.66 (0.52–0.84)
1.39 (0.69–2.79)
Log PSA at diagnosis
<
0.01
1.50 (1.35–1.67)
0.09
1.28 (0.97–1.70)
Clinical T stage
T1 (reference)
0.03
1.00
0.03
1.00
T2
1.26 (1.00–1.58)
1.60 (0.97–2.63)
T3/4
1.56 (1.10–2.21)
2.96 (1.31–6.68)
Primary treatment type
RP (reference)
<
0.01
1.00
Brachytherapy
1.40 (0.94–2.09)
External beam radiation
1.92 (1.45–2.55)
Hormonal therapy
2.58 (1.90–3.50)
AS/WW
2.45 (1.60–3.77)
Clinical site
Academic center
<
0.01
1.00
<
0.01
1.00
Community-based practice
2.65 (1.45–4.86)
2.00 (0.73–5.50)
Veterans Affairs center
2.13 (0.93–4.86)
11.6 (3.01–44.9)
x
2
likelihood ratio
530.3
136.5
RP = radical prostatectomy; HR = hazard ratio; CI = confidence interval; PSA = prostate-specific antigen; AS = active surveillance; WW = watchful waiting.
E U R O P E A N U R O L O G Y 7 1 ( 2 0 1 7 ) 7 5 0 – 7 5 9
752
















