
1.
Introduction
Conceived five decades ago, the Gleason scoring system is a
clinical variable strongly associated with prostate cancer
(PCa) outcome
[1]. With time, incremental modifications to
the standards for pathologic reporting have allowed for
greater agreement between biopsy and radical prostatec-
tomy (RP) specimens, yet have resulted in the elimination of
nearly half of the initially proposed Gleason scores (ie, sums
2–5)
[2–4] .A well-recognized communication challenge
has emerged whereby the lowest assigned Gleason sum
associated with PCa is reported as 6 on a scale from 2 to
10. As a result, a reduction in the practical histologic
spectrum may serve to misrepresent the degree of clinical
risk and potentially compound the problem of overtreat-
ment for men with low-grade tumors with a perceived
higher than actual risk.
A novel grade grouping system offering five tiers
consistent with modern reporting conventions has been
proposed, and there has been a groundswell of momentum
in support of its widespread adoption, including a recent
announcement requiring consistent use for publication in
major urologic oncology journals, including
European
Urology
[5,6]. To date, a number of validation studies
examining the ability of this revised Gleason grading
reporting system to predict clinical recurrence following
definitive therapy have been published, as well as two
publications addressing PCa-specific mortality following
conservative management and radiotherapy
[7–12]. How-
ever, it is unknown if a reporting rubric that collapses the
highest Gleason sums (group V) will in turn mask
differences in clinical outcome within these subcategories,
or whether such a system will perform adequately when
broadly implemented outside of academic centers and
across treatment types. Therefore, we aimed to evaluate the
association of prognostic Gleason grade group with risk of
PCa-specific mortality (PCSM) and the development of bone
metastasis across management strategies among men in a
large multicenter registry.
2.
Patients and methods
Study participants were enrolled in the Cancer of the Prostate Strategic
Urologic Research Endeavor (CaPSURE) registry initiated in 1995, which
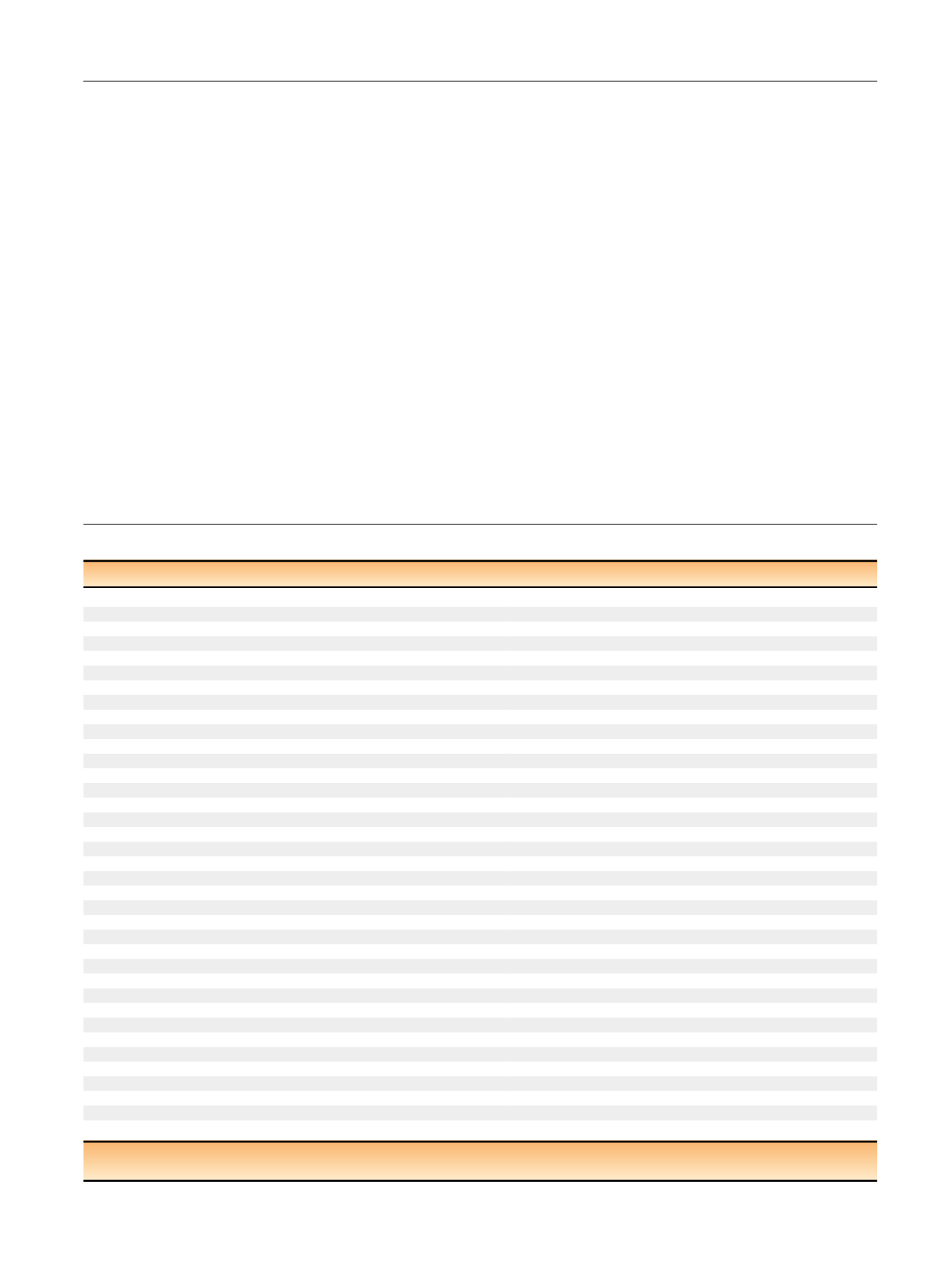
Table 1 – Baseline clinicodemographic and pathologic characteristics among patients with prostate cancer enrolled in CaPSURE
Value
RP
BT
EB
HT
AS/WW
p
value
Mean age, yr (SD)
61.6 (7.0)
68.0 (7.2)
70.1 (6.8)
73.0 (8.3)
71.4 (8.5)
<
0.01
Median PSA, ng/ml (IQR)
5.8 (4.4–8.6)
6.0 (4.6–8.5)
8.4 (5.5–14.8)
10.6 (6.3–23.2)
6.0 (4.4–8.6)
Race/ethnicity,
n
(%)
Native American
17 (
<
1)
0 (0)
2 (
<
1)
2 (
<
1)
0 (0)
<
0.01
Asian/Pacific Islander
25 (
<
1)
4 (
<
1)
10 (1)
19 (1)
7 (1)
Latino/Hispanic
50 (1)
37 (3)
14 (1)
19 (1)
10 (1)
African American
303 (6)
48 (4)
118 (8)
134 (8)
48 (5)
Caucasian
3711 (73)
907 (66)
1040 (67)
953 (60)
646 (67)
Mixed
18 (
<
1)
4 (
<
1)
2 (
<
1)
5 (
<
1)
2 (
<
1)
Other
934 (18)
368 (27)
367 (24)
457 (29)
248 (26)
Clinical T stage,
n
(%)
T1
2486 (51)
688 (53)
624 (42)
631 (42)
567 (63)
<
0.01
T2
2329 (48)
587 (45)
772 (52)
752 (50)
321 (36)
T3
73 (1)
16 (1)
91 (6)
123 (8)
14 (2)
Missing
170
77
66
83
59
Prognostic Gleason group,
n
(%)
I (2–6)
3471 (69)
999 (73)
791 (51)
700 (44)
815 (85)
<
0.01
II (3 + 4)
881 (17)
198 (14)
324 (21)
292 (18)
78 (8)
III (4 + 3)
391 (8)
94 (7)
203 (13)
225 (14)
42 (4)
IV (8)
214 (4)
51 (4)
154 (10)
200 (13)
17 (2)
V (9–10)
101 (2)
26 (2)
81 (5)
172 (11)
9 (1)
Extended Gleason group,
n
(%)
2–6
3471 (69)
999 (73)
791 (51)
700 (44)
815 (85)
<
0.01
3 + 4
881 (17)
198 (14)
324 (21)
292 (18)
78 (8)
4 + 3
391 (8)
94 (7)
203 (13)
225 (14)
42 (4)
4 + 4
181 (4)
36 (3)
132 (9)
152 (10)
14 (1)
3 + 5
25 (
<
1)
15 (1)
16 (1)
36 (2)
3 (
<
1)
5 + 3
8 (
<
1)
0 (0)
6 (
<
1)
12 (1)
0 (0)
4 + 5
63 (1)
13 (1)
42 (3)
103 (7)
4 (
<
1)
5 + 4
20 (
<
1)
6 (
<
1)
19 (1)
34 (2)
2 (
<
1)
10
7 (
<
1)
6 (
<
1)
8 (1)
25 (2)
2 (
<
1)
Missing
11
1
12
10
1
Clinical risk category (CAPRA score),
n
(%)
0–2 (low)
2257 (59)
722 (64)
321 (31)
306 (27)
471 (72)
<
0.01
3–5 (intermediate)
1301 (34)
324 (29)
484 (46)
433 (39)
153 (23)
6–10 (high)
258 (7)
78 (7)
246 (23)
378 (34)
29 (4)
Missing
1242
244
502
472
308
RP = radical prostatectomy; BT = brachytherapy; EB = external beam radiation therapy; HT = hormonal therapy; AS = active surveillance; WW = watchful
waiting; CAPRA = Cancer of the Prostate Risk Assessment.
E U R O P E A N U R O L O G Y 7 1 ( 2 0 1 7 ) 7 5 0 – 7 5 9
751
















