
study revealed that two urodynamic signs commonly
reported by patients with BPS (increased bladder sensation
and painful bladder filling) were more frequent among
patients with BE than in those with a posterior location
only. Furthermore, most of the patients with BE experienced
urgency and/or urinary frequency associated with com-
plaints of bladder pain or bladder pain provoked during
bladder filling, suggesting a direct role of the endometriotic
nodule in the onset of these symptoms/signs. Conversely, it
has been proposed that the presence of BPS in patients with
DIE but without BE is due to modulation of pain responses
by visceral inputs not related to the inflamed site (ie, by
bladder filling when an endometriotic implant is located in
a small part of the bladder wall) as a result of sensitization
[37].
3.2.3.
Questionnaires
In 1992, Barry et al
[50]developed a seven-item question-
naire, the American Urologic Association Symptom Index
(AUASI) (known worldwide as the International Prostate
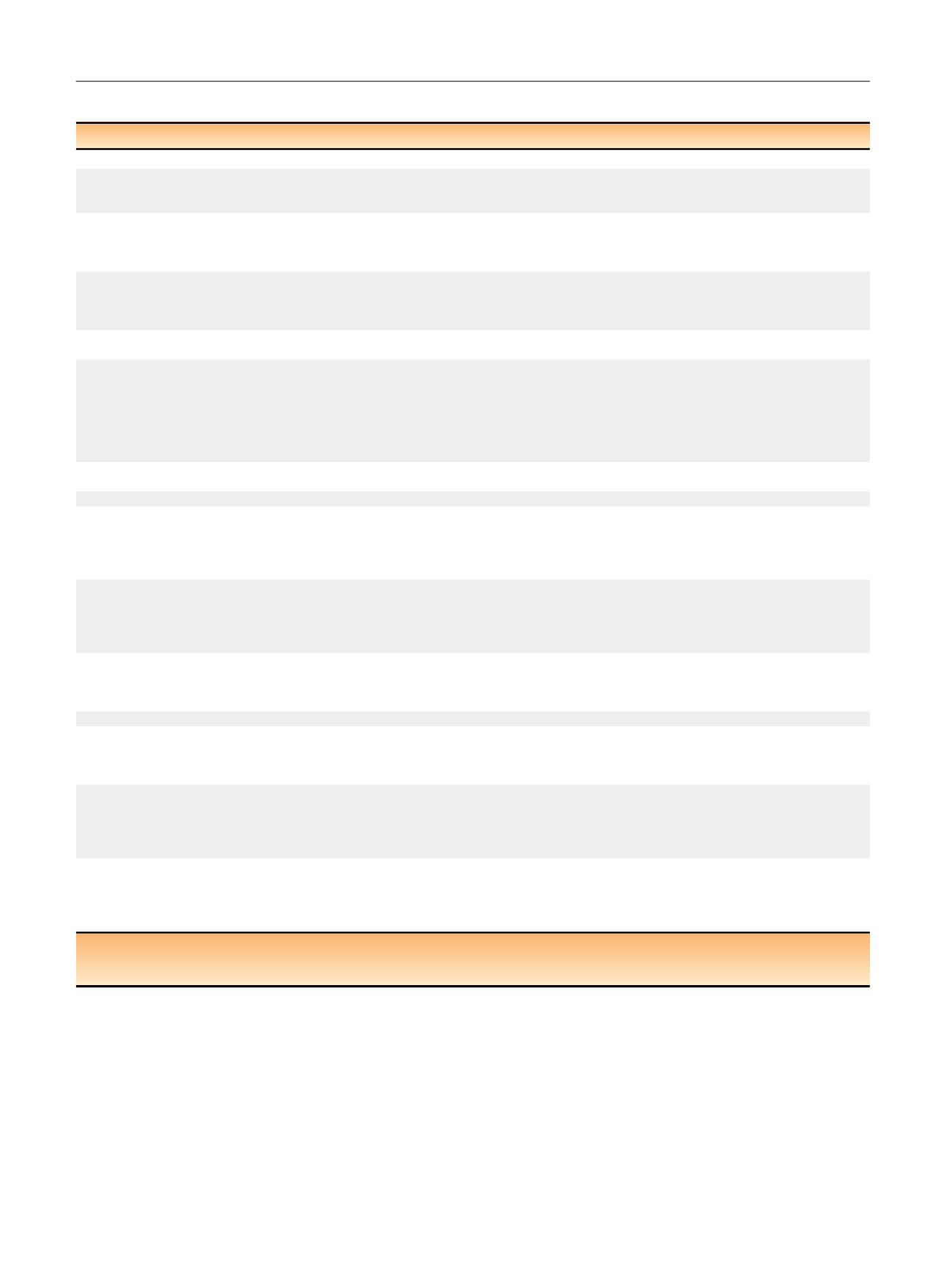
Table 1 – Level of evidence and grade of recommendation for the diagnosis and medical and surgical treatment of bladder endometriosis
Approach
Pros
Cons
Comments
LE
GR
Diagnosis
Physical examination
Noninvasive
Experience required to achieve
accuracy
Allows detection of a bladder
nodule that may be painful
(53–100%)
IIb
B
Questionnaires
Cost-effective, accurate for BE
diagnosis, detailed description
of LUTS
Time-consuming
Can be useful in improving
diagnosis of and monitoring
changes in LUTS after medical/
surgical treatment
IIb
TVS
Highly accurate, noninvasive,
cost-effective, estimation of the
distance between ureteral
orifices and nodule borders
–
First-line technique for BE
diagnosis
Ia
A
MRI
Highly accurate
Not cost-effective
Should not be routinely
performed in clinical practice
Ia
A
Cystoscopy
Cost-effective, estimation of the
distance between ureteral
orifices and nodule borders,
biopsy
Invasive
Should not be performed
routinely, only in cases of
suspicion of malignancy or to
estimate the distance between
ureteral orifices and nodule
borders if not clearly evaluable
by TVS
IV
D
Urodynamics
Objective assessment of lower
urinary tract changes
Invasive, time-consuming
Should only be used for
scientific purposes
III
C
Medical treatment
Combined hormonal
contraceptives and
progestogens
Generally cost-effective,
available in different
formulations (oral, cutaneous,
intrauterine device, implants),
well tolerated
Contraceptive for women
desiring to conceive
First-line therapy
III
C
GnRH-a
Highly effective in improving
symptoms, available in different
formulations (intranasal, IM, SC)
Short-term use (6 mo) without
add-back therapy,
hypoestrogenic AEs, expensive,
contraceptive for women
desiring to conceive
Second-line therapy
III
C
Aromatase inhibitors
Generally effective in improving
symptoms in combination with
hormonal contraceptives,
progestogens
Off-label, high rates of
hypoestrogenic AEs, short-term
use (6 mo)
To be used only in patients
refractory to conventional
therapies and in the setting of
scientific research
III
C
Surgical treatment
TUR
Minimally invasive, fast
recovery (day surgery)
Incomplete lesion removal,
persistence of symptoms, risk of
bladder perforation
Scanty evidence support this
technique that should be used
just in combination with partial
cystectomy
IV
C
Partial cystectomy
Complete lesion removal,
concomitant treatment of other
endometriotic lesions, very low
risk of disease and symptoms
recurrence
Risk of inadvertent removal of
healthy bladder muscle
Simple and safe technique with
excellent long-term efficacy
IIb
B
Combined TUR and
partial cystectomy
Complete lesion removal,
concomitant treatment of other
endometriotic lesions, very low
risk of disease and symptoms
recurrence
Scanty literature based on only
case reports
Combines the advantages of
both techniques
IV
C
LE = level of evidence; GR = grade of recommendation; AEs = adverse events; BE = bladder endometriosis; GnRH-a = gonadotropin releasing hormone agonist;
IM = intramuscular; LUTS = lower urinary tract symptoms; MRI = magnetic resonance imaging; SC = subcutaneous; TUR = transurethral resection;
TVS = transvaginal ultrasonography.
E U R O P E A N U R O L O G Y 7 1 ( 2 0 1 7 ) 7 9 0 – 8 0 7
794
















