
between 1992 and 2007 in order to determine which
parameters predicted competing mortality in this particular
population. Furthermore, we compared the prognostic
impact of individual parameters between patients selected
for radical prostatectomy aged 70 yr or older with their
younger counterparts. Potential prognostic parameters
were obtained from preoperative evaluation records and
discharge letters. Only parameters recorded in at least five
patients were included in the model calculation. Deaths in
the absence of uncontrolled prostate cancer progression or
from unknown causes (
n
= 2) were considered deaths from
competing causes. Demographic data of the study sample
are shown in Supplementary Table 1.
Besides age, five parameters were independent predictors
of competing mortality with hazard ratios of around 2 in
patients aged 70 yr or older
( Table 1). With diabetes mellitus,
chronic lung disease, and other cancer, three common
comorbid conditions independently predicting competing
mortality in younger patients were not thoroughly associat-
ed with competing mortality beyond the 70th yr of age
(Supplementary Table 2). Based on the model obtained in the
latter population, patients were subdivided into quartiles
concerning the parametric part of model-predicted hazards
(Supplementary Fig. 1). Only patients above the fourth
quartile reached the 10-yr mortality rate (29.4%) expected in
the local normal population with the same age structure
(data source:
www.statistik.sachsen.de).
Giving one point for each parameter of the model in
Table 1except for age (ie, for peripheral vascular disease,
cerebrovascular disease, American Society of Anesthesiol-
ogists [ASA] physical status class 3, current smoker, and no
university degree or master craftsman or unknown level of
education as measures for possible occupational or life
style-related risk factors), we calculated a score and
compared it with five other measures of comorbidity for
which data were available in our database (Charlson score,
modified Charlson score, modified Lee mortality index,
prostate cancer specific comorbidity index, and unweighted
Charlson score)
[5–9]. Age was excluded because not all
comparators contained age-related variables and the age
spectrum of patients selected for radical prostatectomy at
an age of 70 yr or older is limited. The score identified in this
study performed best concerning the separation of the
mortality curves (illustrated by the
p
values of comparisons
of neighboring curves) and the Akaike’s information
criterion figures, respectively
( Fig. 1). The obtained simple
score reproduced remarkably well with the multivariable
model and reached narrowly the same Akaike’s information
criterion figure as the stratification into quartiles shown in
Supplementary Figure 1 (1425 vs 1422).
Besides accurate risk prediction, simplicity of use is of
concern with comorbidity classifications in men with early
prostate cancer
[9]. In the suggested score, the five
identified parameters representing different health aspects
may rapidly be assessed during daily clinical practice.
The ability of clinicians to predict life expectancy has
been called into question and available models have not
been considered as better than government life tables
[1]. This study provides arguments for the opposite. In the
subgroup of patients selected for radical prostatectomy
aged 70 yr or older, government life tables would predict a
10-yr mortality rate of 29.4% which corresponds with the
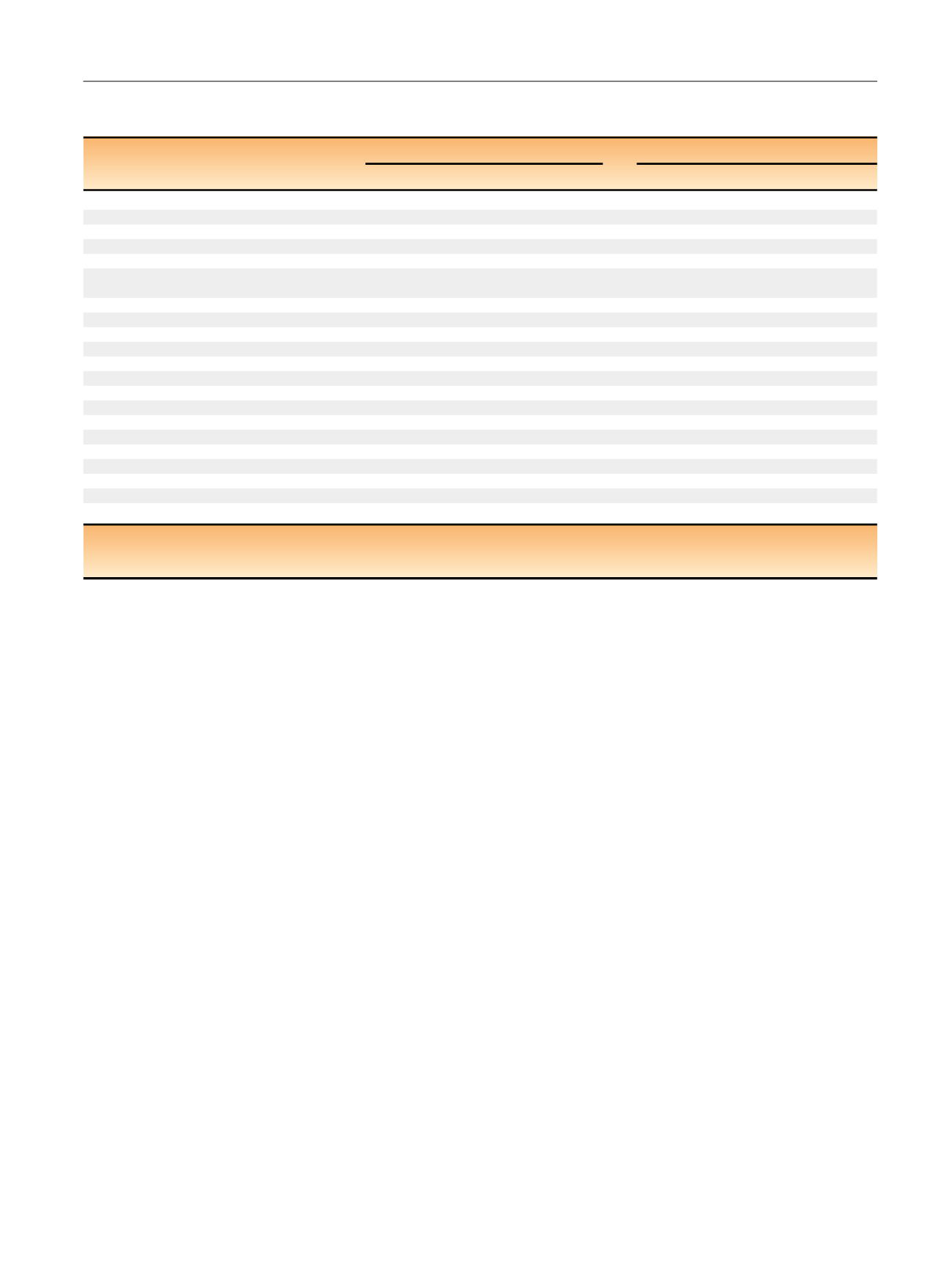
Table 1 – Optimal models predicting competing mortality in patients selected for radical prostatectomy at an age of <70 yr versus those who
underwent surgery at an age of 70 yr or older
<
70 yr (
n
= 2418)
70 yr (
n
= 543)
Category
N
HR
95% CI
p
value
N
HR
95% CI
p
value
Age (continuous variable/yr)
NA
1.12
1.08–1.15
<
0.0001
NA
1.09
1.01-1.18
0.0255
Angina pectoris (CCS classes 2–4 vs 0–1)
99
1.50
1.04–2.17
0.0312
34
Hypertension (vs none)
1240
339
History of thromboembolism (vs none)
75
16
Myocardial infarction (vs none)
98
27
Cardiac insufficiency
(NYHA classes 2–4 versus 0–1)
116
45
Peripheral vascular disease (vs none)
56
2.04
1.35–3.09
0.0007
16
2.33
1.15–4.75
0.0195
Cerebrovascular disease (vs none)
56
24
2.23
1.11–4.47
0.0242
Chronic lung disease (vs none)
233
1.72
1.29–2.28
0.0002
69
Ulcer disease (vs none)
92
19
Diabetes mellitus (vs none)
291
1.58
1.19–2.09
0.0015
91
Connective tissue disease (vs none)
21
1
Hemiplegia (vs none)
2
0
Moderate or severe renal disease (vs none)
26
5.54
3.13–9.81
<
0.0001
8
Solid tumor, leukemia, or lymphoma (vs none)
78
1.69
1.02–2.80
0.0416
20
Liver disease (vs none)
26
8
Dementia (vs none)
1
1
Current smoker (vs ex/nonsmokers)
292
2.06
1.59–2.67
<
0.0001
27
2.18
1.21–3.93
0.0098
Body mass index
<
25 kg/m
2
(vs 25+ kg/m
2
)
668
154
ASA class 3 (versus 1–2)
378
1.63
1.24–2.14
0.0005
134
2.19
1.50–3.21
<
0.0001
No university degree/master craftsma
n a (vs yes)
1372
1.39
1.11–1.74
0.0037
311
2.07
1.41–3.05
0.0002
ASA = American Society Association physical status classification; CCS = Classification of angina pectoris of the Canadian Cardiovascular Society; CI = confidence
interval; HR = hazard ratio; NA = not available; NYHA = Classification of cardiac insufficiency of the New York Heart Association.
a
Unknown.
E U R O P E A N U R O L O G Y 7 1 ( 2 0 1 7 ) 7 1 0 – 7 1 3
711
















