
fourth quartile of the patients in this study (
[3_TD$DIFF]
Supplementary
Fig. 1). Below this level, the parameters identified in this
study enable further detailed risk assessment suggesting
that using clinical and demographic parameters should be
preferred to crude life expectancy prediction based on
government life tables at least in the particularly clinically
critical population of men considered suitable for radical
prostatectomy at an age of 70 yr or older.
Patients undergoing radical prostatectomy are selected
with favorable risks. Therefore, at the same numeric level of
comorbidity, age-adjusted competing mortality rates are
only approximately half as high as in unselected patients
[10] .This selection effect is particularly pronounced beyond
the 70th yr of age
[3] .Obtaining valid predictions of
competing mortality requires taking these facts into
account. All five comorbidity classifications
[5–9]compared
with the newly developed score contained the three
conditions (chronic lung disease, diabetes mellitus, and
other tumors) that were not associated with increased
competing mortality in our sample of elderly patients,
whereas other meaningful parameters (ASA class 3, level of
education, and current smoking) were not included (excep-
tion: current smoking in the Lee mortality index)
[7] .These
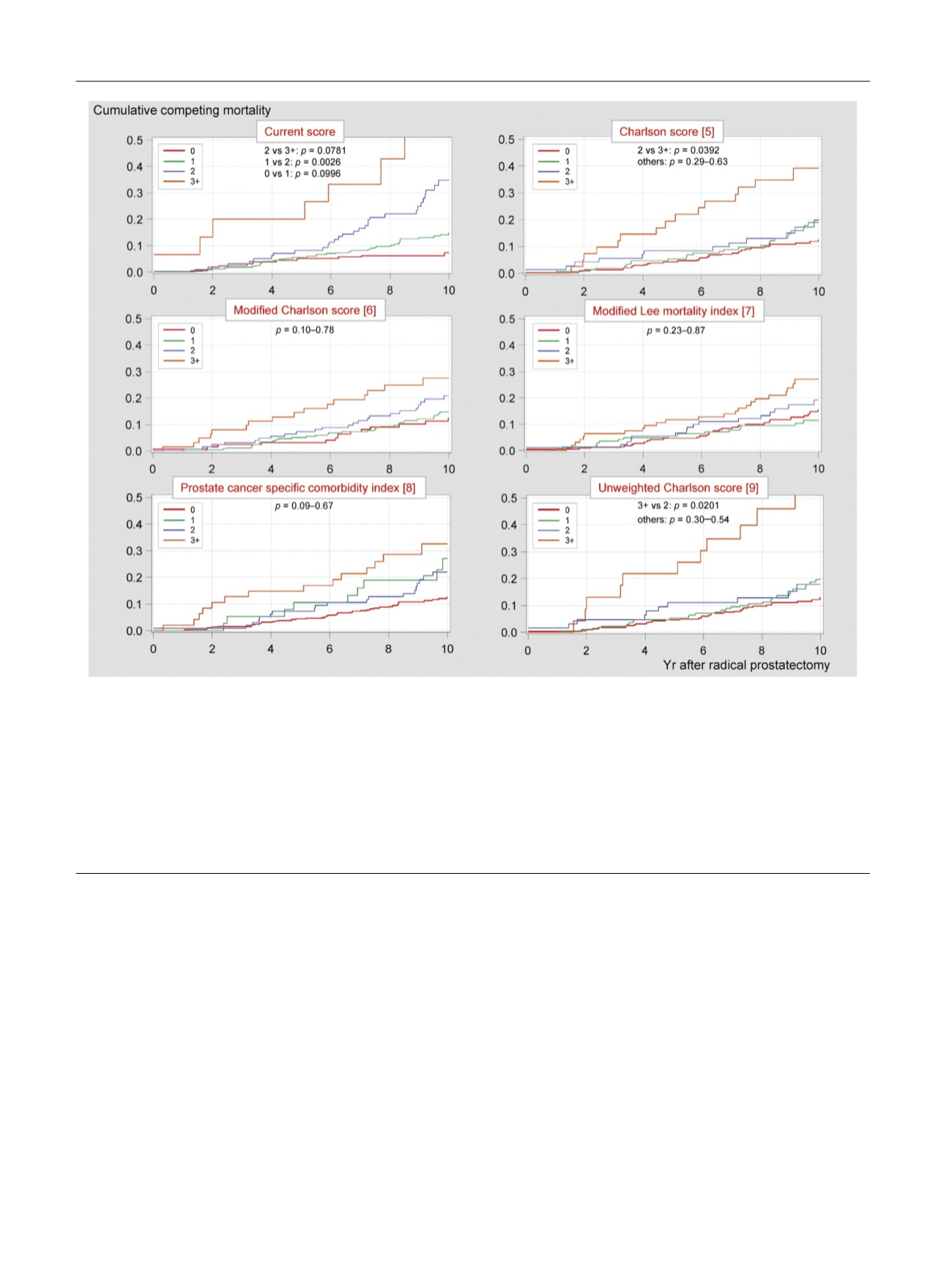
facts could explain the poor separation of the cumulative
mortality curves in the lower risk classes of the compared
comorbidity classifications
( Fig. 1; none of the cumulative
mortality curves of the three lower risk strata differed
significantly from each other in either of the compared
comorbidity measures). The identification of long-living
elderly men is of considerable importance for prostate
cancer screening and for the individualized management of
prostate cancer
[4]. The results of this study suggest that
[(Fig._1)TD$FIG]
Fig. 1 – Cumulative competing mortality curves with Pepe Mori test
p
values and Akaike’s information criterion (lower is better) for the suggested mortality
[1_TD$DIFF]
score (upper diagram in the left column) and five other comorbidity scores using the stratification 0 versus 1 versus 2 versus 3 or more points for all
scores in our sample of 543 patients who underwent radical prostatectomy at an age of 70 yr or older. The Akaike’s information criterion was 1425 for the
current score and ranged between 1452 (unweighted Charlson score) and 1460 (modified Lee mortality index) for the comparators. The following
modifications were made with the tested scores according to the availability of data in our database: (1) modified Charlson score
[6]: data on depression,
Parkinson disease, and multiple sclerosis was not available in our database, these conditions were not considered in calculating this modified Charlson
score, (2) Lee mortality index
[7]: no subdivision between skin cancer and nonskin cancer was made; functional impairments which were not available in
our database and are unlikely of being encountered in candidates for radical prostatectomy were ignored; patients with unknown smoking status were
considered nonsmokers, (3) prostate cancer specific comorbidity index
[8]: other neurological disease, mild renal disease, arrhythmia, valve disease, and
inflammatory bowel disease were not available in our database and were not considered in calculating the index. All cases of chronic lung disease were
considered mild in our study. No subdivision between obstructive and restrictive lung disease was made
[2_TD$DIFF]
. Age-related components in the Lee mortality
index
[7]and the prostate cancer specific comorbidity index
[8]were not used in calculating these scores for comparison.
E U R O P E A N U R O L O G Y 7 1 ( 2 0 1 7 ) 7 1 0 – 7 1 3
712
















