
Partin tables)
[4,5]and analyzed if the addition of MRI
information could improve these clinical models in terms of
pathological outcomes at the time of radical prostatectomy
(RP).
All patients who underwent preoperative 1.5-Tesla MRI
and subsequent RP with pelvic lymph node dissection at
Mayo Clinic Rochester, MN, USA, between 2003 and
2013 were included in this retrospective, Institutional
Review Board approved study. Detailed methods are
reported in Supplementary Data 1. In brief, we used age,
prostate-specific antigen (PSA) at diagnosis, clinical stage
(digital rectal exam), primary and secondary Gleason grade,
Gleason score, percentage of positive/total cores to calculate
Partin Table estimates and CAPRA scores. MRI results for
ECE, SVI, and nodal disease (N+) were collected. Pathological
features (pT, pN, Gleason score, surgical margin status,
SVI, and ECE) were recorded. We developed logistic
multivariable regression models including: clinical vari-
ables (PSA, clinical stage, percentage of involved cores/total
cores, primary Gleason 4–5), Partin Table estimates (for
each specific outcome) and CAPRA scores; MRI results (in
terms of negative/positive exam for each outcome) were
then added in each model and the multivariate modeling
was reassessed. The predictive ability of each model was
further compared developing receiver-operating character-
istic curves and analyzing the area under the curve (AUC)
before and after the addition of MRI.
Five hundred and one patients were included in the final
analysis. Demographic, clinical, and pathological features
are shown in Supplementary Table 1. ECE, SVI, and N+ were
present in 42.3%, 30.7%, and 16.0% of patients, while MRI
results were positive for ECE in 147 patients (29.3%), for SVI
in 83 patients (16.6%), and for N+ disease in 24 (4.8%). As
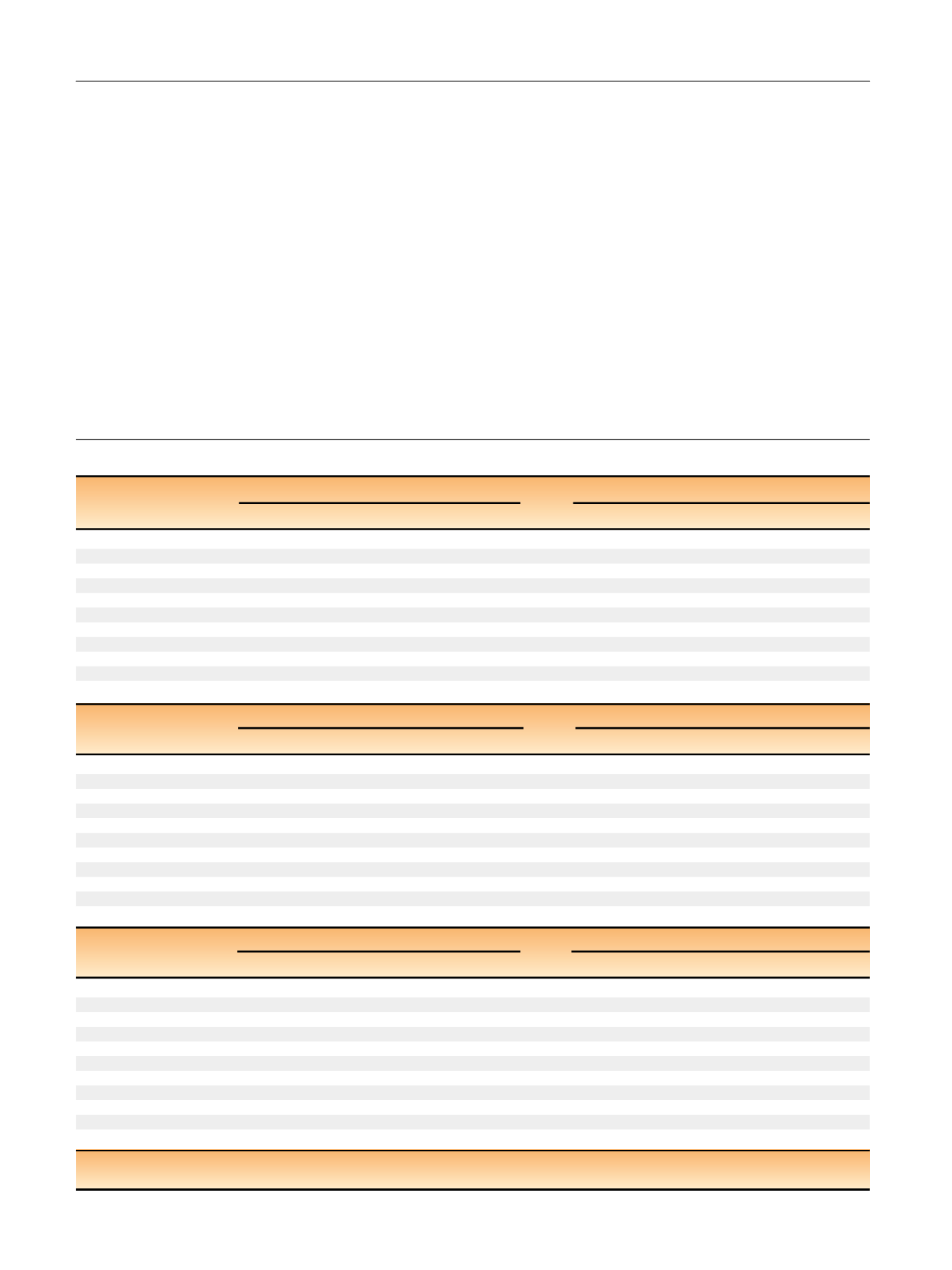
shown in
Table 1, the multivariate clinical models for
Table 1 – Multivariate modeling analysis for predictors of histological outcome
ECE prediction
Without MRI
With MRI
OR
95% CI
p
value
OR
95% CI
p
value
Clinical variables
PSA
1.025
1.000
1.051
0.054
1.021
0.991
1.052
0.173
% core involv.
1.014
1.005
1.023
0.003
1.015
1.004
1.026
0.007
Age at surgery
1.024
0.990
1.060
0.165
1.016
0.976
1.058
0.427
Clinical stage
1.348
1.124
1.616
0.001
1.220
0.975
1.525
0.081
Primary Gleason 4/5
2.344
1.374
4.000
0.002
4.145
2.194
7.833
<
0.0001
MRI ECE result
—
—
—
—
2.379
1.262
4.488
0.007
Partin ECE
1.042
1.019
1.065
0.0003
1.023
0.995
1.052
0.102
MRI ECE result
—
—
—
—
7.522
4.108
13.773
<
.0001
CAPRA score
1.328
1.191
1.481
<
0.0001
1.244
1.095
1.413
0.0008
MRI ECE result
—
—
—
—
5.248
2.994
9.198
<
0.0001
SVI prediction
Without MRI
With MRI
OR
95% CI
p
value
OR
95% CI
p
value
Clinical variables
PSA
1.007
0.983
1.033
0.5572
1.010
0.983
1.038
0.4721
% core involv.
1.026
1.015
1.037
<
0.0001
1.027
1.015
1.040
<
0.0001
Age at surgery
0.997
0.959
1.037
0.8838
0.984
0.940
1.029
0.4768
Clinical stage
1.273
1.048
1.547
0.0148
1.152
0.922
1.441
0.2130
Primary Gleason 4/5
5.707
2.820
11.552
<
0.0001
5.073
2.233
11.524
0.0001
MRI SVI result
—
—
—
—
7.024
3.003
16.431
<
.0001
Partin SVI
1.109
1.075
1.145
<
0.0001
1.098
1.058
1.139
<
0.0001
MRI SVI result
—
—
—
—
7.582
3.449
16.669
<
0.0001
CAPRA score
1.507
1.332
1.706
<
0.0001
1.408
1.222
1.622
<
0.0001
MRI SVI result
—
—
—
—
8.854
4.286
18.288
<
0.0001
N+ prediction
Without MRI
With MRI
OR
95% CI
p
value
OR
95% CI
p
value
Clinical variables
PSA
1.023
0.996
1.051
0.0964
1.032
0.996
1.068
0.0794
% involv core
1.024
1.009
1.039
0.0012
1.020
1.003
1.037
0.0235
Age at surgery
1.003
0.954
1.054
0.9170
0.986
0.928
1.048
0.6558
Clinical stage
1.304
1.025
1.658
0.0304
1.344
1.014
1.782
0.0395
Primary Gleason 4/5
7.147
2.066
24.726
0.0019
9.669
2.263
41.309
0.0022
MRI nodes result
—
—
—
—
4.831
1.320
17.674
0.0173
Partin nodes
1.115
1.074
1.157
<
0.0001
1.102
1.056
1.150
<
0.0001
MRI nodes
—
—
—
—
14.249
3.141
64.638
0.0006
CAPRA score
1.660
1.415
1.948
<
0.0001
1.682
1.392
2.032
<
0.0001
MRI nodes
—
—
—
—
15.060
4.348
52.165
<
0.001
CAPRA = Cancer of the Prostate Risk Assessment; CI = confidence interval; ECE = extracapsular extension; MRI = magnetic resonance imaging; N+ = lymph-node
invasion; OR = odds ratio; PSA = prostate-specific antigen; SVI = seminal vesicle invasion.
E U R O P E A N U R O L O G Y 7 1 ( 2 0 1 7 ) 7 0 1 – 7 0 4
702
















