
tumors, compared to 17 of 126 (14%) ERG-negative tumors,
representing a more than twofold increase in PTEN loss
when ERG expression was present, similar in both groups
( Table 1).
We then evaluated the association between these
alterations and clinical outcomes in the AA population.
The primary outcome was BCR (prostate-specific antigen
0.2 ng/ml), and Cox proportional hazards models were
used for time-to-event analysis. To increase the study
power, we included an additional population of AA men
who underwent RP from 2006 to 2010 with Gleason score
4 + 3 (Supplementary Table 2). Again, higher-grade cancers
were selected to identify the association between these
genomic alterations and clinically relevant disease
[10] .These men were not considered in the prevalence analysis
owing to a lack of matched EA samples. In total, 87 suchmen
were identified and included in a new TMA, of whom 53 had
clinical follow-up, yielding 222 AA men with follow-up for
analysis of outcomes.
The baseline characteristics of the combined AA cohort
are listed in Supplementary Table 3. Some 89 men
experienced BCR. There was no significant interaction
between PTEN and ERG status (
p
= 0.5), and ERG status
was not associated with BCR (HR 1.21, 95% CI 0.74–1.97;
p
= 0.5). In the multivariable model, PTEN loss was
independently associated with higher risk of biochemical
recurrence (HR 2.25, 95% CI 1.33–3.82;
Table 2) in AA men,
as were conventional clinicopathologic factors such as
Gleason score and stage. Given the limited number of
metastatic events (
n
= 22), a full multivariable analysis was
not performed. In a limited model considering PTEN loss
and high-grade cancer (Gleason score 8), however, PTEN
loss was significantly associated with metastases in the AA
population (HR 3.90, 95% CI 1.46–10.4;
p
= 0.007; Supple-
mentary Table 4). Finally, the association between PTEN loss
and BCR did not differ significantly by race when the
original set of 338 matched EA and AA men
( Table 1) was
included in a multivariable model with the same variables
as in
Table 2(interaction term for AA race and PTEN loss, HR
1.45, 95% CI 0.66–3.16;
p
= 0.4).
These data indicate that alterations in both PTEN and
ERG in PCa are significantly less likely among AA
compared to EA men. However, the association between
PTEN loss and higher risk of BCR does not differ
significantly by race and remains similar among AA
men to what has been reported for predominantly EA
cohorts
[6]. In addition, we did not see evidence that ERG
expression is associated with risk of PCa BCR among AA
men, also similar to what has been observed in EA cohorts
[5]. The lower prevalence of PTEN loss among AA tumors
at radical prostatectomy suggests that other molecular
alterations or factors are likely to account for racial
disparities in PCa outcomes. Future work should examine
whether alternative (non–PTEN-mediated) mechanisms
activate PI3K signaling in AA cancers, such as mutations in
PI3K pathway components. Alternatively, it is possible
that altered prevalence of other molecular subtypes, such
as SPINK1 expression and/or
TP53
and
SPOP
mutation, may
contribute to differences in outcome between AA and EA
patients.
The main study limitation is that the population is from a
single tertiary-care institution and may not represent the
general population. However, it is unlikely that this would
affect the population in a race-specific manner. If validated
in additional populations, these data suggest the intriguing
hypothesis that the prevalence, but not the underlying
biology, of the most common PCa molecular subtypes
differs by racial background. Future work will aim to
elucidate whether other molecular alterations contribute to
disparities in PCa outcomes.
Author contributions:
Tamara L. Lotan had full access to all the data in
the study and takes responsibility for the integrity of the data and the
accuracy of the data analysis.
Study concept and design:
Lotan, Schaeffer, Tomlins, Ross, Tosoian, Trock.
Acquisition of data:
Almutairi, Tosoian, Lotan, Hicks, Humphreys, Han,
Sundi, De Marzo
[2_TD$DIFF]
, Morais.
Analysis and interpretation of data:
Lotan, Tosoian, Trock.
Drafting of the manuscript:
Lotan, Tosoian, Almutairi.
Critical revision of the manuscript for important intellectual content:
Schaeffer, Ross, Trock, Sundi.
Statistical analysis:
Tosoian, Trock.
Obtaining funding:
Schaeffer, Lotan.
Administrative, technical, or material support:
Hicks
[3_TD$DIFF]
, Glavaris.
Supervision:
None.
Other:
None.
Financial disclosures:
Tamara L. Lotan certifies that all conflicts of
interest, including specific financial interests and relationships and
affiliations relevant to the subject matter or materials discussed in the
manuscript (eg, employment/affiliation, grants or funding, consultan-
cies, honoraria, stock ownership or options, expert testimony, royalties,
or patents filed, received, or pending), are the following: None.
Funding/Support and role of the sponsor:
This research was funded in
part by an award from the Prostate Cancer Foundation, a CDMRP
Transformative Impact Award (W81XWH-12-PCRP-TIA), and NIH Cancer
Center Support Grant 5P30CA006973-52. The sponsors played a role in
data collection.
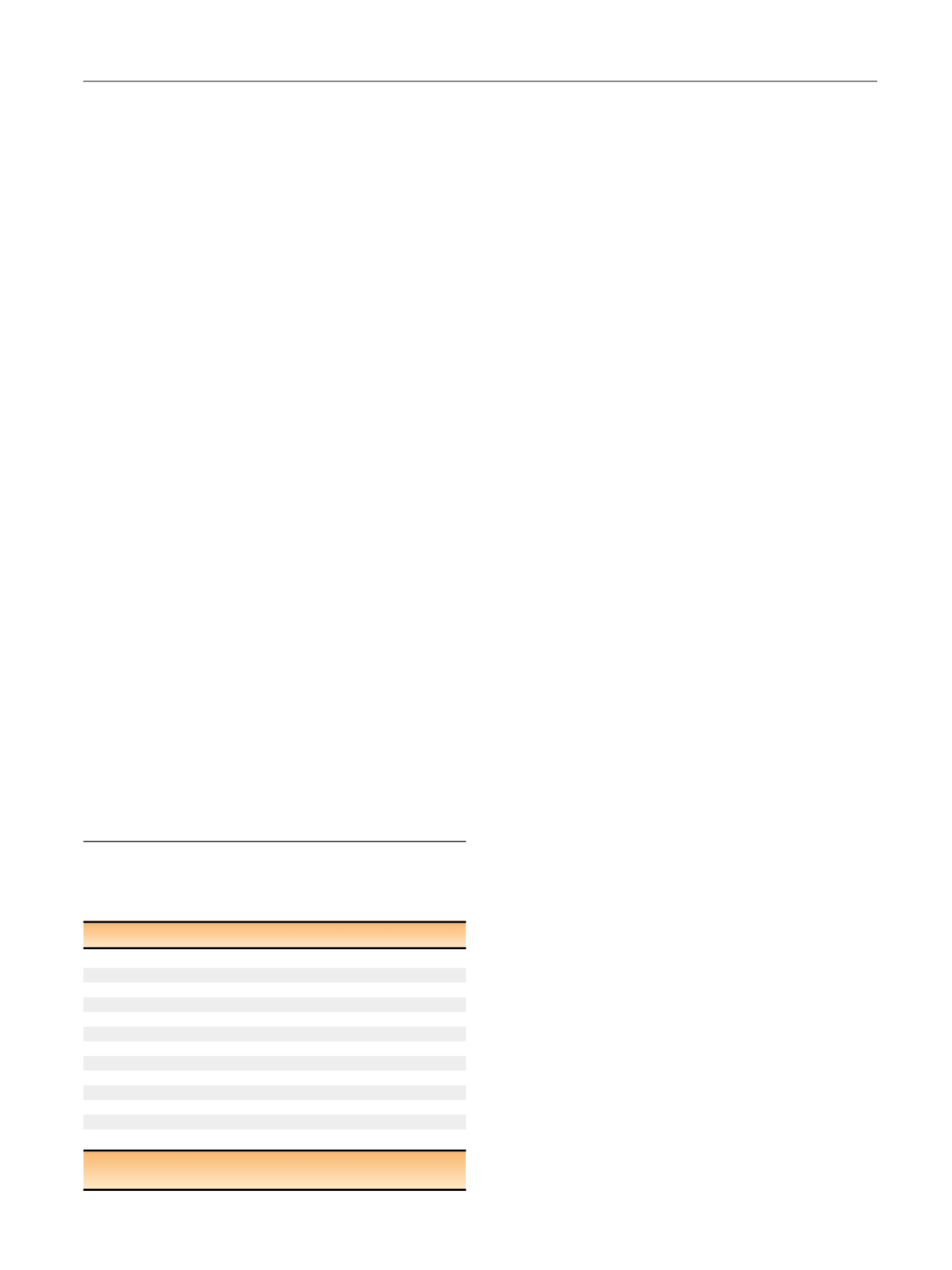
Table 2 – Multivariable Cox proportional hazard models assessing
association of clinicopathologic parameters and PTEN/ERG status
with biochemical recurrence in the combined African-American
prostate cancer cohort (
n
= 222)
Variable
Multivariable HR (95% CI)
p
value
Prostate-specific antigen
1.01 (0.99–1.04)
0.4
RP grade group
1 (GS 6)
1.00 (reference)
2 (GS 3 + 4)
2.16 (0.90–5.23)
0.086
3 (GS 4 + 3)
5.02 (1.92–13.1)
0.001
4 (GS 8)
5.45 (2.03–14.6)
0.001
5 (GS 9–10)
4.03 (1.39–11.9)
0.011
Pathologic stage
T2N0
1.00 (reference)
T3aN0
1.89 (1.03–3.57)
0.041
T3bN0
3.14 (1.56–6.30)
0.001
N1
6.64 (2.92–15.1)
<
0.001
PTEN loss
2.25 (1.33–3.82)
0.003
HR = hazard ratio; CI = confidence interval; RP = radical prostatectomy;
GS = Gleason score.
E U R O P E A N U R O L O G Y 7 1 ( 2 0 1 7 ) 6 9 7 – 7 0 0
699
















