
4.
Discussion
This is the largest comparative study of outcomes exclu-
sively for patients with bGS 9–10 CaP. After adjusting for
age, clinical stage, bGS, initial PSA, year of treatment, and
use of salvage therapies, 5-yr and 10-yr CSS and OS rates
were similar across all three cohorts. We also found that
5-yr and 10-yr DMFS rates are significantly improved with
EBRT + BT when compared with either EBRT or RP. Thus, our
data suggest that EBRT-based treatments and RP are at least
equivalent for the treatment of bGS 9–10 CaP, with
extremely dose-escalated RT potentially offering the best
systemic control.
The equivalence of CSS and OS following EBRT-based
treatments and RP in our series differs from the majority of
prior comparative studies
[4–7]. Importantly, the majority
of EBRT patients in prior studies received neither long-
course ADT nor high-dose RT. In contrast, the majority of RT
patients treated in our series were treated in accordance
with contemporary standards. Nearly 94% of EBRT patients
had upfront ADT with a median duration of 24 mo and 97%
of EBRT patients received doses isoeffective to, or higher
than, 75.6 Gy in 1.8-Gy fractions (the high-dose arm in a
randomized trial demonstrating a systemic control benefit
to dose-escalation)
[10] .On subset analyses, the total
radiation dose was associated with improved long-term
outcomes—an effect likely driven by the EBRT + BT cohort.
An inability to identify an effect for ADT duration might be
related to the homogeneity of ADT duration within the EBRT
and EBRT + BT cohorts, and given the small numbers of
patients who received no ADT or short-term ADT, our study
may not have been powered to detect an effect from ADT
duration. Thus, our data suggest that comparisons between
RP and substandard EBRT techniques should be regarded
with caution.
Several other details warrant consideration. Firstly,
post-RP BCRs are diagnosed at a lower PSA threshold than
post-RT BCRs, introducing bias when comparing frequency.
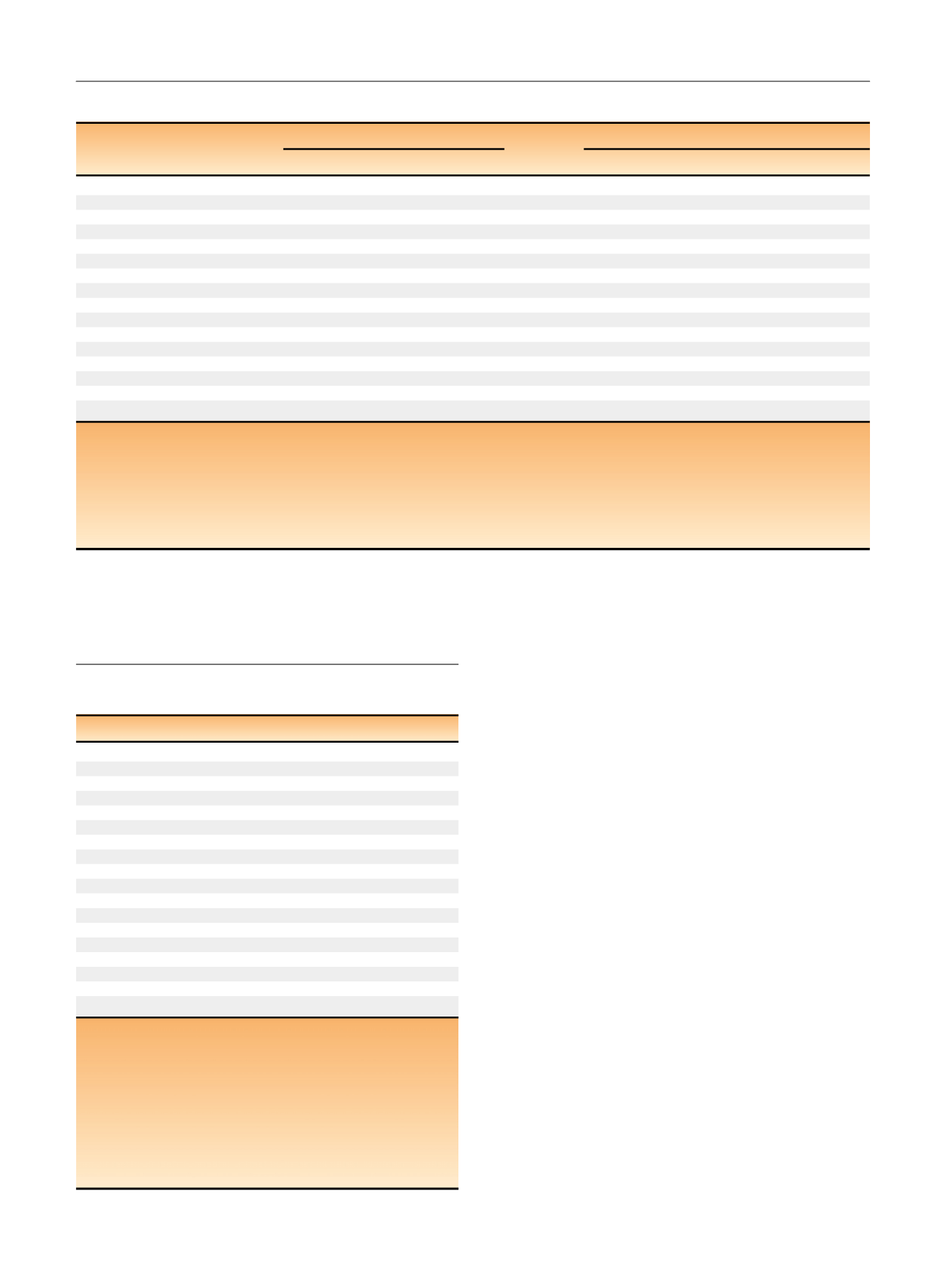
Table 3 – Kaplan-Meier analysis and multivariate Cox regression of clinical outcomes.
Kaplan-Meier analysi
s aMultivariate Cox regression
Clinical outcome
5-yr
10-yr
HR
95% CI
p
value
Biochemical recurrence
EBRT vs RP (%)
28.2% vs 73.
6 a39.7% vs 83.
8 b0.21
(0.14, 0.32)
<
0.0001
EBRT + BT vs EBRT (%)
17.1% vs 28.2
30.0% vs 39.7
0.76
(0.44, 1.32)
0.33
EBRT + BT vs RP (%)
17.1% vs 73.
6 a30.0% vs 83.
8 b0.16
(0.09, 0.28)
<
0.0001
Distant metastasis
EBRT vs RP (%)
21.3 vs 20.9
33.3 vs 38.5
0.78
(0.45, 1.35)
0.37
EBRT + BT vs EBRT (%)
5.4 vs 21.
3 a10.2 vs 33.
3 a0.30
(0.12, 0.72)
0.008
EBRT + BT vs RP (%)
5.4 vs 20.
9 a10.2 vs 38.
5 a0.23
(0.09, 0.6)
0.003
Prostate cancer specific mortality
EBRT vs RP (%)
8.4%vs 8.3
19.5 vs 21.5
0.75
(0.34, 1.65)
0.47
EBRT + BT vs EBRT (%)
4.4 vs 8.4
11.9 vs 19.5
0.64
(0.24, 1.71)
0.37
EBRT + BT vs RP (%)
4.4 vs 8.3
11.9 vs 21.5
0.48
(0.16, 1.4)
0.18
Overall survival
EBRT vs RP (%)
79.9 vs 90.3
65.3 vs 72.1
1.07
(0.58, 1.98)
0.82
EBRT + BT vs EBRT (%)
84.7 vs 79.9
59.2 vs 65.3
0.99
(0.58, 1.69)
0.98
EBRT + BT vs RP (%)
84.7 vs 90.3
59.2 vs 72.1
1.06
(0.53, 2.12)
0.86
CI = confidence interval; BT = brachytherapy; EBRT = external beam radiotherapy; HR = hazard ratio; RP = radical prostatectomy; RT = radiotherapy.
a
The Kaplan-Meier analysis was not adjusted for age, Gleason score, clinical T stage, or initial prostate-specific antigen, and comparisons between cohorts
was performed using the log-rank test. The multivariate Cox regression model derived-hazard ratios are adjusted for age, Gleason score, clinical T-stage,
initial prostate-specific antigen, year of treatment, local salvage (with time to salvage as a covariate), and systemic salvage (with time to salvage as a
covariate) and refer to outcomes through 10 yr of follow-up (Cox analysis for outcomes through 5 yr of follow-up can be found in Supplementary
Table 2).
For example, a hazard ratio
<
1 for the comparison external beam radiotherapy versus radical prostatectomy suggests that the given outcome (eg,
biochemical recurrence) has a lower hazard of occurring with external beam radiotherapy versus with radical prostatectomy.
b
These comparisons showed statistically significant differences on Kaplan-Meier survival analysis.
Table 4 – Multivariate Cox regression of clinical outcomes by
subgroups.
Clinical outcome
HR
95% CI
p
value
Biochemical recurrenc
e aTotal RT dose
0.95
(0.91, 0.98)
0.0043
ADT duration
1.00
(0.99, 1.01)
0.48
Distant metastasis
Total RT dose
0.91
(0.87, 0.96)
0.0001
ADT duration
1.01
(1, 1.02)
0.26
Salvage RT
0.47
(0.19, 1.15)
0.099
Adjuvant RT
0.86
(0.2, 3.72)
0.84
Prostate cancer specific mortality
Total RT dose
0.93
(0.87, 0.99)
0.020
ADT duration
1.01
(1, 1.02)
0.051
Salvage RT
0.53
(0.19, 1.5)
0.23
Adjuvant RT
0.55
(0.07, 4.23)
0.57
Overall survival
Total RT dose
0.98
(0.95, 1.01)
0.23
ADT duration
1.00
(0.99, 1.01)
0.53
Salvage RT
0.47
(0.19, 1.15)
0.099
Adjuvant RT
0.86
(0.2, 3.72)
0.84
ADT = androgen deprivation therapy; CI = confidence interval; HR = hazard
ratio; RT = radiotherapy.
a
The multivariate Cox regression model derived-hazard ratios are
adjusted for age, Gleason score, clinical T-stage, and initial prostate-specific
antigen, year of treatment, local salvage (with time to salvage as a
covariate), and systemic salvage (with time to salvage as a covariate) and
refer to outcomes through 10 yr of follow-up. Hazard ratios
<
1 suggest the
outcome (eg, distant metastasis) has a lower hazard of occurring with
higher values of continuous variables (total radiotherapy dose or androgen
deprivation therapy duration) or ‘‘yes’’ for binary variables (salvage
radiotherapy or adjuvant radiotherapy).
E U R O P E A N U R O L O G Y 7 1 ( 2 0 1 7 ) 7 6 6 – 7 7 3
770
















