
3.
Results
3.1.
Patient and primary treatment characteristics
Patient and treatment characteristics are presented in
Tables 1 and 2, respectively. The median follow-up of the
overall cohort was 4.6 yr (interquartile range [IQR], 2.87–
7.36 yr). Median follow-up lengths were 4.2 (IQR, 2.78–
6.25) yr, 6.5 (IQR, 3.16–9.19) yr, and 4.9 (IQR, 4.26–8.90) yr
for EBRT, EBRT + BT, and RP patients. There were no
significant differences between follow-up durations.
Patients in the EBRT and EBRT + BT cohorts had higher
age, initial PSAs, and clinical stages than patients in the RP
cohort (
p
<
0.05). Two hundred and sixteen (93.9%) EBRT
and 75 (86.2%) EBRT + BT patients had upfront ADT. The
duration of ADT was significantly longer in the EBRT cohort
(median of 24 mo vs 8 mo,
p
<
0.05). Pelvic nodal irradiation
was performed in similar percentages of EBRT and
EBRT + BT patients (76.1% and 78.2%, respectively,
p
>
0.5). In order to compare different dose/fractionation
regimens, doses were converted into equivalent doses in
2-Gy fractions (EQD
2
s), assuming an alpha/beta ratio of
1.5
[24]. The median EQD
2
for EBRT patients was 76.4 Gy
(65–80 Gy), compared with 88.7 Gy (81.9–98.9 Gy) for
EBRT + BT patients (
p
<
0.0001). HDR-BT boosts were
24 Gy in six fractions by
192
Ir, while LDR-BT boosts were
108 Gy by
125
I.
Fifty-eight patients undergoing RP (34.1%) had robotic-
assisted RPs. One hundred and forty one RP patients had
available first postoperative PSAs, among which 33 (23.4%)
had PSAs 0.2 ng/ml. Of these, 29 (87.9%) ultimately
received SRT. Considerable pathologic upstaging was found
(
p
<
0.0001). Thirty-six (21.2%) patients had pathologic GS
7–8 CaP. Notably, 21 (58%) of these patients still had a
component of Grade 5 CaP either as the primary or
secondary grade
[6] ,or as the tertiary grade
[15].
3.2.
Adjuvant and salvage treatments
Twenty-one RP patients (12.4%) had adjuvant radiation
therapy (ART). Of RP patients with BCRs but no DMs at time
of BCR, 85.3% received SRT. Nine RP patients (5.3%) had
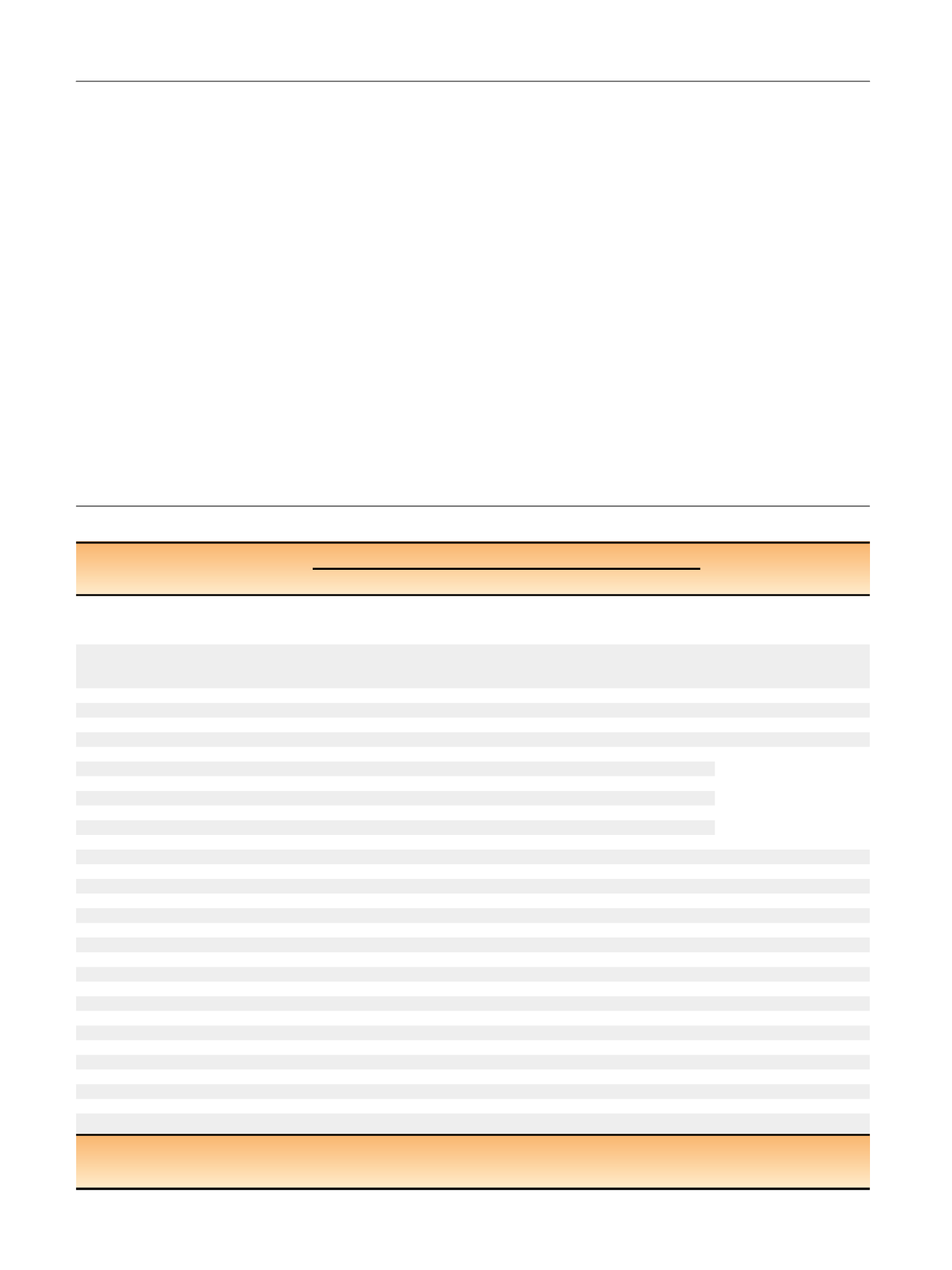
Table 1 – Clinical and pathologic characteristics.
Treatment cohort
EBRT (
n
= 230)
EBRT + BT (
n
= 87)
RP (
n
= 170)
p
value
Age, mean, median (range yr)
69.9
70 (43–98)
69.1
70 (50–82)
61.9
62 (42–77)
>
0.5 (EBRT vs EBRT + BT)
<
0.0001 (RP vs EBRT)
<
0.0001 (RP vs EBRT + BT)
Initial PSA, mean, median (range ng/ml)
18.7
9.76 (0.54–270)
16.7
11.7 (1.7–95.2)
11.5
7.8 (0.4–124)
>
0.1 (EBRT vs EBRT + BT)
<
0.001 (RP vs EBRT + BT)
<
0.01 (RP vs EBRT)
Biopsy Gleason Score
9
208 (90.4)
82 (94.3)
161 (94.7)
>
0.1
10
22 (9.6)
5 (5.7)
9 (5.3)
Clinical stage,
n
(%)
1c
71 (29.6)
17 (19.5)
95 (55.9)
<
0.05 (EBRT vs EBRT + BT)
<
0.0001 (RP vs EBRT)
<
0.0001 (RP vs EBRT + BT)
2a
41 (17.8)
14 (16.1)
27 (15.9)
2b
25 (10.7)
20 (23.0)
20 (11.8)
2c
17 (7.4)
2 (2.3)
7 (4.1%
3a
38 (16.5)
13 (14.9)
13 (7.7)
3b
11 (4.9)
8 (9.2)
2 (1.2)
4
27 (11.8)
13 (14.9)
6 (3.5)
Pathological stage,
n
(%)
2a
13 (7.6)
2b
3 (1.8)
2c
21 (12.4)
3a
39 (17.7)
3b
81 (47.7)
4
22 (12.9)
Pathological Gleason Scor
e a , n(%)
7
20 (11.8)
8
16 (9.4)
9
128 (75.2)
10
6 (3.5)
Adverse pathologic features,
n
(%)
Positive margins
69 (40.6)
pN+
28 (16.5)
Treatment center,
n
(%)
UCLA
132 (57.4)
20 (23)
145 (85.3)
CET
67 (77)
FCC
98 (42.6)
25 (14.7)
BT = brachytherapy; CET = California Endocurie Therapy Center; EBRT = external beam radiotherapy; FCC = Fox Chase Cancer Center; pN+ = positive nodes on
lymph node dissection; PSA = prostate-specific antigen; RP = radical prostatectomy; UCLA = University of California, Los Angeles.
a
Two patients had androgen deprivation therapy effect preventing Gleason scoring at radical prostatectomy.
E U R O P E A N U R O L O G Y 7 1 ( 2 0 1 7 ) 7 6 6 – 7 7 3
768
















