
Radical cystectomy with extended pelvic lymph node
dissection (PLND) provides the best chance of long-term
survival for clinically localised muscle-invasive bladder
cancer and high-grade recurrent noninvasive disease
[1].
However, curative surgery remains challenging, with recur-
rence rates of 30–40% reported within 5 yr of surgery
[2].
Recurrences often occur early; more than 80% occur within
the first 2 yr after surgery, with average presentation
occurring 10–15 mo after radical cystectomy
[3].
Debate remains as to whether minimally invasive
surgery negatively impacts survival outcomes due to
inadequate resection, suboptimal lymph node dissection,
or alteration of recurrence patterns due to tumour seeding
related to pneumoperitoneum or insufflation
[4] .A recent
single-centre study compared open radical cystectomy
(ORC) with robot-assisted radical cystectomy (RARC) and
reported a similar incidence of overall transitional cell
carcinoma (TCC) recurrences, with a higher frequency of
peritoneal carcinomatosis and extraperitoneal lymph node
recurrences among patients undergoing RARC
[4].
It is recognised in ORC series that early recurrence is an
indicator of poor prognosis that correlates closely with 5-yr
recurrence-free survival (RFS) and overall survival
[5] .The
current evidence for long-term outcomes following RARC
shows acceptable oncologic outcomes comparable to open
series
[2]. A multicentre study analysing data for 702 RARC
patients with a minimum of 5-yr follow-up (median 67 mo)
reported 5-yr RFS of 67%.
In the European Association of Urology Robotic Urology
Section (ERUS) Scientific Working Group database,
717 patients at nine different institutions were identified
who underwent totally intracorporeal RARC between
December 2003 and March 2015. The follow-up protocol
comprised history, physical examination, urine cytology,
and laboratory measurements according to EAU guidelines.
Diagnostic imaging was routinely performed at 4–6 mo for
the first year, and at least annually thereafter, or more
frequently when clinically indicated. The median follow-up
was 31 mo (interquartile range [IQR] 20–46).
Patient demographics and oncologic outcomes are
summarised in
Table 1. Thirty-four patients (4.8%) had a
positive surgical margin (PSM), of whom 31 (4.4%) had pT3/
T4 disease. Three patients (0.4%) with organ-confined
disease had a PSM. The median yield for extended PLND
was 18 (IQR 13–25). Kaplan-Meier estimates were created
for local and distant recurrence sites
( Table 2 ). RFS at 3, 12,
and 24 mo was 95.9%, 80.2%, and 74.6% respectively
(Supplementary Fig. 1). Univariable and multivariable Cox
regression was used to estimate hazard ratios for predictors
of RFS (Supplementary material).
We observed early recurrences at any site in 4.1% of
patients at 3mo, 19.8% at 12mo, and 25.4% at 24mo, similar
to rates seen in ORC series
[5–7] .Distant recurrences were
most frequent in the bones, lungs, and liver, while local
recurrences were most common in pelvic lymph nodes.
This is consistent with recurrence patterns seen in ORC and
in autopsy series
[6,7]. Regarding unusual recurrence
patterns
[4], five patients (0.7%) had peritoneal carcino-
matosis and two patients (0.3%) had metastasis at the port
site (wound site), which are both of low incidence and
consistent with published ORC series
[7]. In a recent
review, RFS rates at 2 yr after surgery ranged from 67% to
81% in RARC series
[8], and studies highlighting unusual
recurrence patterns as a possible indicator of a detrimental
effect have not shown a higher incidence of recurrences
compared to ORC performed in the same institution
[4].
It has been found at autopsy that peritoneal carcinoma-
tosis incidence is as high as 19% among bladder cancer
patients, but importantly it is most frequently associated
with extensive metastases at multiple sites
[6] .Review of
the patients in our series with peritoneal carcinomatosis
and port-site metastasis revealed that all had high-grade
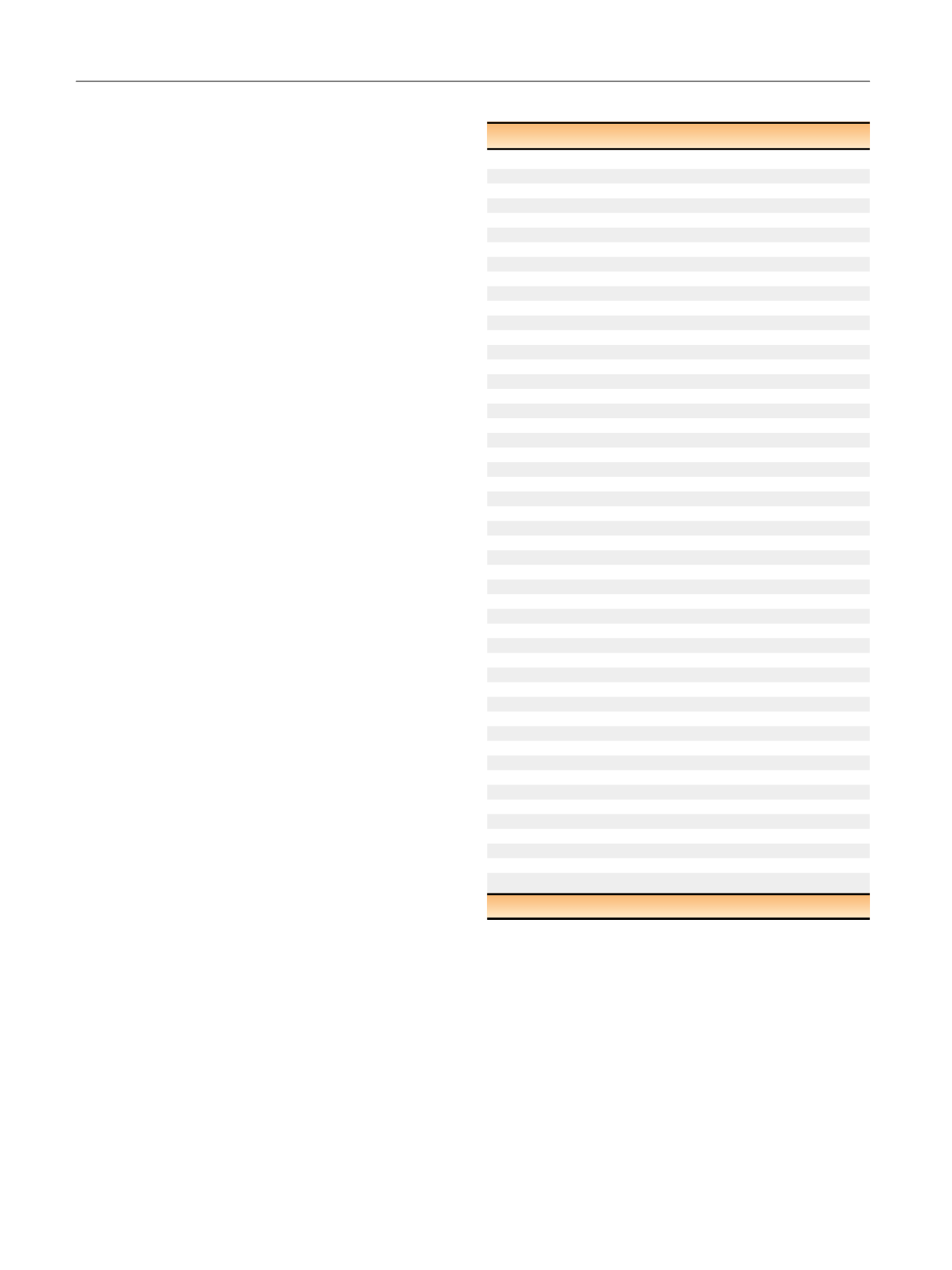
Table 1 – Patient demographics and oncologic outcomes
Variable
Result
Patients (n)
717
Male/female (
n
)
78/22
Median age, yr (IQR)
68 (62–74)
ASA grade (
n
)
1
17
2
51
3
31
4
1
Median BMI, kg/m
2
(IQR)
26 (23–28)
Median follow-up, mo (IQR)
31 (20–46)
Histology,
n
(%)
Transitional cell carcinoma
680 (95.2)
Squamous cell carcinoma
20 (2.8)
Adenocarcinoma
9 (1.2)
Neuroendocrine
2 (0.3)
Small cell carcinoma
3 (0.4)
Missing data
3
Preoperative staging,
n
(%)
Carcinoma in situ
34 (4.8)
Ta
25 (3.5)
T1
154 (21.6)
T2
370 (52.0)
T3
76 (10.7)
T4
19 (2.7)
Non–transitional cell carcinoma
34 (4.8)
Missing data
5
Received neoadjuvant chemotherapy,
n
(%)
176 (25.2)
Missing data
19
Pathological stage (%)
pT0
136 (19.1)
pTis
76 (10.7)
pTa
34 (4.8)
pT1
72 (10.1)
pT2
162 (22.7)
pT3
163 (22.9)
pT4
69 (9.7)
Missing data
5
Soft tissue margin positive,
n
(%)
34 (4.8)
Missing data
2
PLND template,
n
(%)
No PLND
35 (5.1)
Standard
144 (20.8)
Extended PLND
518 (74.3)
Missing
20
Pathologic nodal stage,
n
(%)
Nx
35 (4.9)
N0
548 (77.1)
N1
58 (8.2)
N2
70 (9.8)
Missing
6
PLND = pelvic lymph node dissection.
E U R O P E A N U R O L O G Y 7 1 ( 2 0 1 7 ) 7 2 3 – 7 2 6
724
















