
ratio [AOR] for RP: 0.873, 95% confidence interval [CI]:
0.872–0.874, per yr). Increasing Charlson comorbidity score
was associated with a higher likelihood of receiving RP
(AOR: 1.65, 95% CI: 1.62–1.68, for score 1 and AOR: 1.42,
95%CI: 1.37–1.48, for score 2,
p
<
0.001). Race was
independently associated with treatment modality, with
[25_TD$DIFF]
non-White patients significantly less likely to receive RP
(AOR: 0.49, 95% CI: 0.48–0.50, for Blacks and AOR: 0.92, 95%
CI: 0.89–0.95, for Hispanics,
p
both
<
0.001). Uninsured
patients and those with Medicaid were less likely to receive
RP (AOR: 0.61, 95% CI: 0.57–0.64, for the uninsured and
AOR: 0.50, 95% CI: 0.48–0.52, for Medicaid patients vs those
with private insurance,
p
both
<
0.001) while patients aged
65 yr or older with Medicare were slightly more likely to
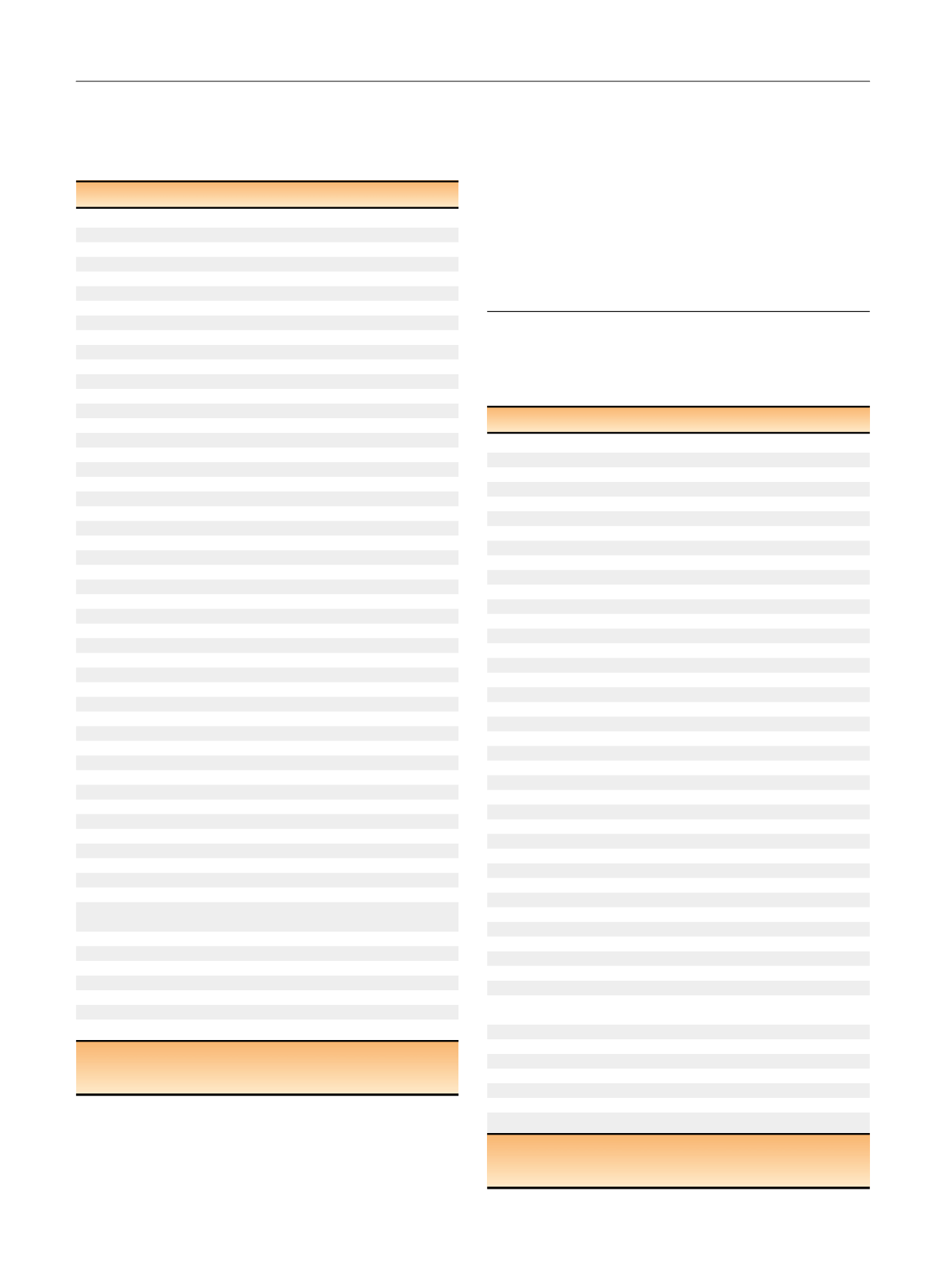
Table 2 – Multivariate logistic regression model of factors
associated with treatment received for those receiving radical
prostatectomy versus radiation therapy (external beam
radiotherapy or brachytherapy). A higher adjusted odds ratio (AOR)
indicates a higher likelihood of receiving radical prostatectomy
Variable
AOR (95% CI)
p
value
Age (yr)
0.87 (0.87–0.87)
<
0.001
Race
Non-Hispanic White
1
Hispanic
0.92 (0.89–0.95)
<
0.001
Black
0.49 (0.48–0.50)
<
0.001
Other
0.89 (0.85–0.92)
<
0.001
Insurance typ
e aPrivate
1
Uninsured
0.61(0.57–0.64)
<
0.001
Medicaid
0.50 (0.48–0.52)
<
0.001
Younger Medicare
0.58 (0.56–0.60)
<
0.001
Older Medicare
1.03 (1.01–1.05)
0.003
Government
0.14 (0.13–0.15)
<
0.001
Diagnosis year
2004
1
2005
1.06 (1.03–1.09)
<
0.001
2006
1.20 (1.16–1.23)
<
0.001
2007
1.45 (1.41–1.49)
<
0.001
2008
1.92 (1.87–1.98)
<
0.001
2009
2.10 (2.04–2.16)
<
0.001
2010
2.41 (2.34–2.48)
<
0.001
2011
2.56 (2.49–2.64)
<
0.001
2012
2.56 (2.49–2.64)
<
0.001
Modified Charlson comorbidity score
0
1
1
1.65 (1.62–1.68)
<
0.001
2
1.42 (1.37–1.48)
<
0.001
Clinical T stage
T3/T4
1
T2
1.21 (1.16–1.26)
<
0.001
T1
1.15 (1.10–1.20)
<
0.001
Combined Gleason score
8–10
1
7
1.46 (1.43–1.50)
<
0.001
2–6
0.86 (0.84–0.88)
<
0.001
Prostate specific antigen level
>
20 ng/ml
1
10–20 ng/ml
1.32 (1.28–1.36)
<
0.001
<
10 ng/ml
1.84 (1.80–1.89)
<
0.001
Income level
$46 000
1
$35 000–45 999
0.97 (0.96–0.99)
<
0.001
$30 000–34 999
0.92 (0.90–0.94)
<
0.001
<
$30 000
0.84 (0.83–0.86)
<
0.001
Treatment facility type
NCI network cancer center
1
Teaching/research hospital
0.36 (0.35–0.37)
<
0.001
Comprehensive community
cancer program
0.27 (0.27–0.28)
<
0.001
Community cancer program 0.19 (0.18–0.19)
<
0.001
Other
0.29 (0.29–0.30)
<
0.001
US census region
Northeast
1
Midwest
1.42 (1.39–1.44)
<
0.001
South
1.38 (1.36–1.41)
<
0.001
West
1.64 (1.60–1.67)
<
0.001
CI = confidence interval; NCI = National Cancer Institute.
a
Younger Medicare refers to patients aged 18–64 yr receiving Medicare
coverage while Older Medicare refers to those aged 65 yr or older.
Table 3 – Multivariate logistic regression model of factors
associated with receiving observation versus definitive local
treatment (radical prostatectomy, radiation therapy, cryotherapy)
for patients with low-risk prostate cancer. A higher adjusted odds
ratio (AOR) indicates a higher likelihood of receiving observation
Variable
AOR (95% CI)
p
value
Age (yr)
1.08 (1.08–1.08)
<
0.001
Race
Non–Hispanic White
1
Hispanic
1.08 (1.00–1.15)
0.04
Black
1.26 (1.21–1.31)
<
0.001
Other
1.02 (0.94–1.11)
0.6
Insurance type
Private
1
Uninsured
2.87 (2.61–3.15)
<
0.001
Medicaid
1.88 (1.72–2.06)
<
0.001
Younger Medicare
1.50 (1.41–1.60)
<
0.001
Older Medicare
0.96 (0.93–1.00)
0.03
Government
0.55 (0.45–0.67)
<
0.001
Diagnosis year
2004
1
2005
1.08 (1.01–1.15)
0.03
2006
1.06 (0.99–1.13)
0.1
2007
1.05 (0.98–1.11)
0.2
2008
1.29 (1.21–1.37)
<
0.001
2009
1.88 (1.77–1.99)
<
0.001
2010
1.84 (1.73–1.95)
<
0.001
2011
2.33 (2.20–2.46)
<
0.001
2012
3.17 (2.99–3.37)
<
0.001
Modified Charlson comorbidity score
0
1
1
0.87 (0.84–0.91)
<
0.001
2
1.30 (1.21–1.40)
<
0.001
Clinical T stage
T1
1
T2
0.71 (0.68–0.74)
<
0.001
Income level
$46 000
1
$35 000–45 999
1.02 (0.99–1.06)
0.2
$30 000–34 999
1.03 (0.99–1.07)
0.1
<
$30 000
[8_TD$DIFF]
1.06 (
[9_TD$DIFF]
1.01–
[10_TD$DIFF]
1.11)
[11_TD$DIFF]
0.02
Treatment facility type
NCI network cancer center
1
Teaching/research hospital
[12_TD$DIFF]
0.55 (
[13_TD$DIFF]
0.52–
[14_TD$DIFF]
0.57)
<
0.001
Comprehensive community
cancer program
0.36 (0.35–0.37)
<
0.001
Community cancer program
[15_TD$DIFF]
0.59 (
[16_TD$DIFF]
0.56–
[17_TD$DIFF]
0.62)
<
0.001
Other
0.36 (0.34–0.38)
<
0.001
US census region
Northeast
1
Midwest
0.85 (0.82–0.88)
<
0.001
South
0.86 (0.83–0.89)
<
0.001
West
1.19 (1.14–1.24)
<
0.001
CI = confidence interval; NCI = National Cancer Institute.
a
Younger Medicare refers to patients aged 18–64 yr receiving Medicare
coverage while Older Medicare refers to those aged 65 yr or older.
E U R O P E A N U R O L O G Y 7 1 ( 2 0 1 7 ) 7 2 9 – 7 3 7
734
















